The Consequences of In vitro Fertilization Treatment
Maryam Farzaneh*
Department of Stem Cells and Developmental Biology, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- *Corresponding Author:
- Maryam Farzaneh
Department of Stem Cells and Developmental Biology,
Ahvaz Jundishapur University of Medical Sciences, Ahvaz,
Iran,
Tel: 9104579736;
Email: maryamfarzaneh2013@yahoo.com
Received: May 4, 2020, Manuscript No. ipjcs-20-3979 Editor assigned: May 7, 2020, PreQC No. ipjcs-20-3979; Reviewed: May 21, 2020, QCNo. ipjcs-20-3979; Revised: June 28, 2022, QI No. ipjcs-20-3979; Manuscript No. R-26601; Published: July 26, 2022, DOI: 10.21767/2471-9749.2022.7.5.152
Citation: Farzaneh M (2022) The Consequences of In vitro Fertilization Treatment. J Reproduct Health Contracept Vol: 7 No: 5:152.
Abstract
Infertility as a disease of the reproductive system is the inability to become pregnant after 12 months of intercourse without contraception using no birth control methods. In vitro Fertilization (IVF) as a form of Assisted Reproductive Technology (ART) and the most effective intervention is used to treat infertility issues with the joining of a woman's egg and a man's sperm outside the body, in a laboratory. There are several steps including hormonal stimulation, egg retrieval, insemination, fertilization, embryo culture, and embryo transfer to the woman's body. If the chance of fertilization is low, in Intra Cytoplasmic Sperm Injection (ICSI) procedure the sperm is directly injected into the cytoplasm of an egg. IVF as a breakthrough in the treatment of infertility provides the best opportunity of having a child using their own eggs. IVF can be more successful than other forms of ART such as Intrauterine Insemination (IUI) method. Although the procedure of IVF has many advantages for a couple who would be unable to have a baby, it has some disadvantages. The review aims to update the potential impact and risks at different times in the IVF process.
https://betsatgirisi.com https://bettilte.com https://vegabete.com https://kanyongiris.com https://matgiris.com https://celtabetegiris.com https://hilbetegiris.com https://melbete.com https://kinbettinge.com https://wipbett.com https://pusulabetegiris.com https://superbahiss.com https://lidyagiris.com https://holiganbete.com https://1xbetgiriss.com https://asyabahise.com https://jetbahise.com https://betdoksana.com https://betebetle.com https://betgramagiris.com
Keywords
Infertility; In vitro fertilization; Pregnancy; Embryo culture; Advantages; Disadvantages
Introduction
Infertility as a disease of the reproductive system is biological inability to achieve pregnancy after 12 months or more of unprotected intercourse [1]. The development of In vitro Fertilization (IVF) improved the management of female infertility and used to overcome reproductive problems [2,3]. IVF is a complex series of procedures used to treat infertility issues or prevent genetic disorders [4,5]. IVF as a form of Assisted Reproductive Technology (ART) and a major breakthrough in embryo transfer is the joining of a woman's egg and a man's sperm outside the body, in vitro “in glass” [6]. In 1978, the first ‘IVF baby’ was born using natural IVF by Louise Brown [7]. Since then, IVF outcomes improved and provided large numbers of women the possibility of becoming pregnant and increased their chances [8,9]. In traditional IVF, 50,000 or more swimming sperm are placed next to the egg in an environmentally controlled chamber in a laboratory [10]. Fertilization is the process in which one of the sperm is placed next to the egg to form a diploid cell, known as zygote [11,12].
In the IVF, there are several steps including hormonal stimulation or superovulation with exogenous gonadotropins or similar substances to release more than one healthy egg in a month, egg retrieval or follicular aspiration after a minor surgery, In vitro Maturation (IVM) of gametes, insemination or inserting the highest quality sperm with the best quality eggs, fertilization, embryo culture or cleavage-stage embryos, preimplantation genetic diagnosis, and embryo transfer to the woman's uterus [13,14]. If the chance of fertilization is low, in Intra Cytoplasmic Sperm Injection (ICSI) procedure the sperm being directly injected into the cytoplasm of an egg with a micropipette to promote fertilization [15,16]. After traditional IVF or ICSI, once sperm-egg fusion happens, the fertilized egg or an embryo is cultured for 2-6 days and transferred to the same or another woman’s womb [17,18] (Figure 1).After fertility treatment, at the same time, more than one embryo may be put into the uterus of a female [19]. Embryo Transfer (ET) number is dependent on the various variables such as maternal age and egg quality and fertility [20]. Although the procedure of IVF has many advantages for a couple who would be unable to have a baby, it has some disadvantages. This review aims to update the potential impact and risks at different times in the IVF process.
Literature Review
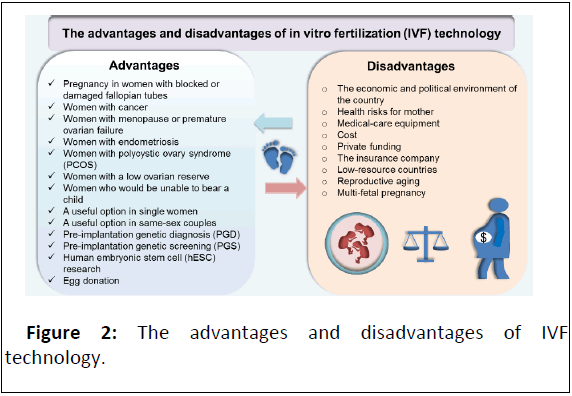
With the advent of ART, IVF as a breakthrough in the treatment of infertility provides the best opportunity of having a child using their own eggs [21]. The advantage of IVF is achieving a successful pregnancy in women with blocked or damaged fallopian tubes, in unexplained or undiagnosed infertility, management for women with cancer, women with menopause or premature ovarian failure, women with endometriosis, patients with Polycystic Ovary Syndrome (PCOS), and patients with a low ovarian reserve or people who would be unable to bear a child [22,23]. Male factor infertility will exhibit a much higher chance of the live birth IVF success rate than in other cases of IVF [24,25]. IVF can be more successful than other forms of ART such as Intrauterine Insemination (IUI) method that involves putting sperm directly into a woman's cervix, fallopian tubes, or uterus to facilitate fertilization [26,27]. IUI can be a useful option for single women and same couples to become parents. If IUI has not been successful, IVF with donor sperm can provide a great opportunity for helping couples who wish to have a child [28-30]. IVF with fewer drugs can decrease the risk of side effects in some patients who are at high risk for Ovarian Hyper Stimulation Syndrome (OHSS) [31-33]. IVF with Pre-implantation Genetic Diagnosis (PGD) and Pre-implantation Genetic Screening (PGS) can also help to find out fertilization problems and inherited diseases such as cystic fibrosis, Huntington’s Disease (HD), Down’s syndrome, and muscular dystrophy to improve the chances of a successful outcome [34,35]. With the permission of the biological parents, unused embryos can be donated for human Embryonic Stem Cell (hESC) research, or to help other people who would be unable to have a baby [36-40]. Therefore, IVF is the most powerful fertility treatment available that can help couples overcome various types of infertility and give patients a good chance of success (Figure 1).
In the IVF, there are several steps including hormonal stimulation to release more than one healthy egg in a month, putting a needle through vaginal wall and into the ovary for egg retrieval, insemination or inserting the highest quality sperm with the best quality eggs, fertilization, embryo culture and embryo transfer to the woman's womb [41]. If the chance of fertilization is low, in Intra Cytoplasmic Sperm Injection (ICSI) procedure the sperm is directly injected into the cytoplasm of an egg with a micropipette to promote fertilization (Figure 2).
Discussion
Multiple variables such as the economic and political environment of the country, the education and reproductive health care level, and medical-care equipment at the hospital can be important to accessing IVF treatment [42]. Despite the development of IVF more than 30 years ago, the cost as an important element and a barrier to accessing IVF treatment remains high. IVF is an expensive treatment in most parts of the world. The average cost of one fresh IVF cycle in the United States costs around $12,000. If patients require further ART, the cost will be higher as much as $15,000 via private funding. IVF treatment in the United Kingdom and Australia costs per IVF/ICSI cycles is around $5,000-6,000 that is available in a range of prices [43]. IVF in developing countries is limited to people who can afford the cost involved. In resource-poor countries, a large majority of the population cannot afford infertility treatment; because the insurance company only covered fertility diagnosis, not treatment. In recent years, there has been growing interest in finding strategies to enhance the level of mother care in lowresource countries [44,45].
Therefore, the development of low-cost and cost-effective IVF treatment is urgent in areas with limited resources. Public funding (full, partial) and the provision of health insurance for IVF treatment can remove the remaining barrier to IVF by covering fertility care or egg-freezing [46]. There are several strategies to reduce cost in IVF including simplifying diagnostics methods, decreasing the cost of ovarian stimulation, reducing fertility drug levels, simplifying the IVF procedures, and decreasing the need for sophisticated IVF related equipment in the laboratory. Research has shown that IVF is not an effective treatment due to reproductive aging and has low success rates less than 20% per cycle in women 40 and beyond [47]. So, these patients by using their own oocytes do not benefit from ART procedures. Although IVF side effects will vary depending upon the patient, multi-fetal pregnancy or the risk of multiple births should be considered as an adverse effect of IVF for infertility treatment. Therefore, critical attention would be necessary to improve treatment fertilization problems.
Conclusion
To date, IVF has increased the treatment of infertility and used to overcome reproductive problems or prevent genetic disorders. Several basic issues and interventions need to be elucidated to facilitate effective IVF treatment, especially for individuals of lower socioeconomic backgrounds who cannot afford many of the health care. IVF, unlike other medical procedures, is still too expensive for most and the management of each condition presents many challenges.
Declaration of Interest
The authors declare no conflict of inte rest.
References
- Kukla R (2019) Infertility, epistemic risk, and disease definitions. Synthese 196: 4409-4428.
- Ben-Ami I, Raziel A, Gidoni Y, Fauser BC, Ron-El R (2017) Indications for in vitro fertilization treatment From diagnosis to prognosis. Textbook of Assisted Reproductive Techniques. CRC Press.
- Somigliana E, Vigano P, Benaglia L, Busnelli A, Berlanda N, et al. (2017) Management of endometriosis in the infertile patient. Semin Reproduct Med 35: 31-37.
- Donnez J, Dolmans MM (2017) Fertility preservation in women. New Engl J Med 377: 1657-1665.
- Goel NJ, Meyers LL, Frangos M (2018) Pseudohypoparathyroidism type 1B in a patient conceived by in vitro fertilization: Another imprinting disorder reported with assisted reproductive technology. J Assist Reprod Genet 35: 975-979.
- Kamel RM (2013) Assisted reproductive technology after the birth of Louise Brown. J Reprod Infertility 14: 96.
- Talmor A, Dunphy B (2015) Female obesity and infertility. Best Pract Res Clin Obstet Gynaecol 29: 498-506.
- Velez MP, Hamel C, Hutton B, Gaudet L, Walker M, et al. (2019) Care plans for women pregnant using assisted reproductive technologies: A systematic review. Reprod Health 16: 1-19.
- Cohen J (2018) Animal track to human assisted in-vitro reproduction: Fertilization. In-Vitro Fertilizat Pioneers' Hist 8.
- Rao KA (2018) The infertility manual. JP Medical Ltd.
- Frederiksen Y, Mehlsen MY, Matthiesen SM, Zachariae R, Ingerslev HJ (2017) Predictors of pain during oocyte retrieval. J Psychosom Obstet Gynecol 38: 21-29.
- Golestanfar A, Shirazi A, Shams-Esfandabadi N, Ahmadi E (2017) Using effective compounds on sperm chromatin structure in intracytoplasmic sperm injection (ICSI) procedure. Iran J Vet Clin Sci 11.
- Roychoudhury S, Maldonado‐Rosas I, Agarwal A, Esteves SC, Henkel R, et al. (2018) Human sperm handling in intracytoplasmic sperm injection processes: In vitro studies on mouse oocyte activation, embryo development competence and sperm oxidation-reduction potential. Andrologia 50: e12943.
- Eltoukhi NM, Azzam HF, Hani M, Abdel-Monem AS (2017) Relationship between women's body mass index and success rate of in vitro fertilization. Malaysian J Med Res 1: 8-17.
- Tanveer A, Malviya N, Yadav D (2018) Omics approaches in in vitro fertilization. Omics Technol Bio-Eng.
- Wintner EM, Hershko-Klement A, Tzadikevitch K, Ghetler Y, Gonen O, et al. (2017) Does the transfer of a poor quality embryo together with a good quality embryo affect the in vitro fertilization (IVF) outcome?. J Ovarian Res 10: 1-5.
- Grondahl ML, Christiansen SL, Kesmodel US, Agerholm IE, Lemmen JG, et al. (2017) Effect of women’s age on embryo morphology, cleavage rate and competence-a multicenter cohort study. PLoS One 2: e0172456.
- Harwood K (2009) Egg freezing: A breakthrough for reproductive autonomy? Bioethics 23: 39-46.
- Zhang M, Bu T, Tian H, Li X, Wang D, et al. (2019) Use of cumulative live birth rate per total number of embryos to calculate the success of IVF in consecutive IVF cycles in women aged ≥ 35 years. Bio Med Res Int 2019.
- Tan J, Tannus S, Taskin O, Kan A, Albert AY, et al. (2019) The effect of unilateral tubal block diagnosed by hysterosalpingogram on clinical pregnancy rate in intrauterine insemination cycles: Systematic review and meta‐analysis. BJOG: Int J Obstet Gynaecol 126: 227-235.
- Provost MP, Acharya KS, Acharya CR, Yeh JS, Steward RG, et al. (2016) Pregnancy outcomes decline with increasing body mass index: Analysis of 239,127 fresh autologous in vitro fertilization cycles from the 2008-2010 society for assisted reproductive technology registry. Fertil Steril 105: 663-669.
- Klonoff-Cohen HS (2017) Prevailing knowledge about male and female lifestyle habits and in vitro fertilization in the 21st century. Med Res Arch 5.
- Atalay E, Ozaksit MG, Tokmak A, Engin-Ustun Y (2019) Intrauterine insemination versus timed intercourse in ovulation induction cycles with clomiphene citrate for polycystic ovary syndrome: A retrospective cohort study. J Gynecol Obstet Human Reprod 48: 805-809.
- Pekcan MK, Kokanali D, Kokanali K, Tasci Y (2018) Effect of time intervals from the end of sperm collection to intrauterine insemination on the pregnancy rates in controlled ovarian hyperstimulation-intrauterine insemination cycles. J Gynecol Obstet Human Reprod 47: 561-564.
- Feldberg D (2017) Fertility treatment and preservation in transgender men and women. Principles Gender-Specific Med.
- Dauod L, Schenker JG (2018) Ovarian hyperstimulation syndrome (OHSS): Pathogenesis and prevention. Reprod Med Clin Pract.
- Toftager M, Bogstad J, Bryndorf T, Lossl K, Rosker J, et al. (2016) Risk of severe ovarian hyperstimulation syndrome in GnRH antagonist versus GnRH agonist protocol: RCT including 1050 first IVF/ICSI cycles. Hum Reprod 31: 1253-1264.
- Malhotra N, Gupta S, Malhotra J, Goswami D, Bora NM, et al. (2018) Merits and demerits of in vitro fertilization in batches. Pract Guide Assist Reprod Technol 21.
- Georgiou EX, Melo P, Baker PE, Sallam HN, Arici A, et al. (2019) Long‐term GnRH agonist therapy before in vitro fertilisation (IVF) for improving fertility outcomes in women with endometriosis. Cochrane Database Syst Rev 11.
- Dorscheidt J, Repping S (2018) The position of the unborn in human embryo research. Children’s Rights Health Care.
- Farzaneh M, Alishahi M, Derakhshan Z, Sarani NH, Attari F, et al. (2019) The expression and functional roles of miRNAs in embryonic and lineage-specific stem cells. Curr Stem Cell Res Ther 14: 278-289.
- Kolagar TA, Farzaneh M, Nikkar N, Khoshnam SE (2020) Human pluripotent stem cells in neurodegenerative diseases: Potentials, advances and limitations. Curr Stem Cell Res Ther 15: 102-110.
- Farzaneh M, Derakhshan Z, Hallajzadeh J, Sarani NH, Nejabatdoust A, et al. (2019) Suppression of TGF-β and ERK signaling pathways as a new strategy to provide rodent and non-rodent pluripotent stem cells. Curr Stem Cell Res Ther 14: 466-473.
- Teoh PJ, Maheshwari A (2014) Low-cost in vitro fertilization: Current insights. Int J Women's Health 6: 817.
- Gerrits T (2012) Biomedical infertility care in low resource countries: Barriers and access. Facts Views Vis Obgyn Monog 2: 1-6.
- Ombelet W (2011) Global access to infertility care in developing countries: A case of human rights, equity and social justice. Facts Views Vision Obgyn 3: 257.
- Ombelet W, Campo R (2007) Affordable IVF for developing countries. Reprod Biomed Online 15: 257-265.
- Zhang X, Zhuxiao R, Xu F, Zhang Q, Yang H, et al. (2018) Congenital tuberculosis after in vitro fertilization: Suggestion for tuberculosis tests in infertile women in developing countries. J Int Med Res 46: 5316-5321.
- Ombelet W, Cooke I, Dyer S, Serour G, Devroey P (2008) Infertility and the provision of infertility medical services in developing countries. Human Reprod Update 14: 605-621.
- Ombelet W, Goossens J (2017) Global reproductive health-Why do we persist in neglecting the undeniable problem of childlessness in resource-poor countries?. Facts Views Vis Obgyn 9: 1.
- Blerkom JV, Hennigan C, Ombelet W (2019) Design and development of simplified, low-cost technologies for clinical IVF: Applications in high-and low-resource settings. In Vitro Fertilizat.
- Fauser BC (2019) Towards the global coverage of a unified registry of IVF outcomes. Reprod Biomed Online 38: 133-137.
- Connolly MP, Pollard MS, Hoorens S, Kaplan BR, Oskowitz SP, et al. (2008) Long-term economic benefits attributed to IVF-conceived children: A lifetime tax calculation. Am J Manag Care 14: 598-604.
- Feichtinger M, Nordenhok E, Olofsson JI, Hadziosmanovic N, Rodriguez-Wallberg KA (2019) Endometriosis and cumulative live birth rate after fresh and frozen IVF cycles with single embryo transfer in young women: No impact beyond reduced ovarian sensitivity-a case control study. J Assist Reprod Genet 36: 1649-1656.
- Reljic M, Lovrec VG (2019) Predictive factors for live birth in autologous in vitro fertilization cycles in women aged 40 years and older. Sloven J Public Health 58: 173-178.
- Pinzauti S, Ferrata C, Vannuccini S, Di Rienzo G, Severi FM, et al. (2016) Twin pregnancies after assisted reproductive technologies: The role of maternal age on pregnancy outcome. Euro J Obstet Gynecol Reprod Biol 206: 198-203.
- Velez MP, Hamel C, Hutton B, Gaudet L, Walker M, et al. (2019) Care plans for women pregnant using assisted reproductive technologies: A systematic review. Reprod Health 16: 1-19.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences