Presentation and Intervention in Missing Copper T Thread in Reference to Timingof Insertion
Pooja Rani, Alka Sehgal, Dilpreet Kaur Pandher, Bikramjit Singh Jafra
Published Date: 2021-10-22Pooja Rani*1, Alka Sehgal2, Dilpreet Kaur Pandher3, Bikramjit Singh Jafra4
1Department of MS, DNB Obstetrics and gynecology, Specialist medical officer, civil hospital, Mohali, India
2Department of MD, DNB, MNAMS, Obstetrics and gynaecology, Govt. Medical College and Hospital, Sector-32, Chandigarh, India
3Department of MD, Obstetrics and gynaecology, Professor, Govt. Medical College and Hospital, Sector-32, Chandigarh, India
4Department of DNB, Pediatrics, Assistant Professor, Gyan Sagar Medical College and Hospital, Rajpura, India
- *Corresponding Author:
- Rani P
Department of MS, DNB obstetrics and gynecology, Specialist medical officer. Civil hospital, Mohali, India
Tel: 8284074961
E-mail:drpooja01234@gmail.com
Received Date: July 28, 2021; Accepted Date: October 12, 2021; Published Date: October 22, 2021
Citation: Rani P, Sehgal A, Pandher K D, Jafra S B (2021) Presentation and Intervention in Missing Copper T Thread in Reference to Timing of Insertion, J Contracept Stud, Vol: 6 No: 1
Abstract
Objective
To analyse the impact of time of insertion of Copper T to presentation and intervention for management of missing Cu-T thread.
Methodology and setting
One year data of 57 patients, referred, reported or detected with missing Cu T thread collected. Retrospective data was collected from OT and OPD hospital records and duly completed telephonically.
Outcomes measured
Data was analysed with various interrelated factors like relation to timing of insertion, presentation, complications, number and kind of interventions for its removal.
Type of statistical analysis
Proportion of women with missing Cu T thread were calculated among all women in percentages. Correlation between different groups couldn’t be calculated because of major difference in the number of subjects in groups.
Results
Among 57 women, 30 had post LSCS Cu T insertion, 6 had post NVD, 20 had interval Cu T insertion and 1 had post abortal insertion. Misplaced Cu T was detected in 8 women on USG, 4(50%) had post LSCS, 3(37.5%) post NVD and 1(12.5%) had interval Cu T insertion. OPD removal could be attempted successfully in 30 women; 11(36.67%) post LSCS, 2 (33.33%) post NVD, 16(80%) interval and 1(100%) post abortion insertion. OT removal was needed in 23 women, (17 (56.67%) post LSCS, 2(33.33%) post NVD, 4(20%) interval Cu T insertion). Spontaneous expulsion diagnosed in 4, 2 post LSCS and 2 post NVD Cu T insertion.
Conclusion
There is definite impact of timing of Cu T insertion on incidence of misplacement and expulsion and more studies and data is needed for developing a common information performa to develop SOPs for follow up of such patients.
Keywords
IUCD – Intrauterine Contraceptive Device; Cu T – Copper T; SOP- Standard operating procedure; hysteroscopy; missing Cu T Thread
Introduction
Copper T (Cu T) is an IUCD and a long-acting reversible contraceptive (LARC) method with many major advantages like noninterference with sexual intercourse, better efficacy (pearl index = 0.83), good compliance and easy to follow up. In India, where the population stood at more than 1.2 billion at the last count, population explosion is at its worst and family planning is the need of the hour [1]. Considering the matter as serious since 1952, India was the first country in the world to launch a National Programme for Family Planning. Since then, this program has undergone many transformations in terms of policy and actual program implementation. The optimum utilisation is yet to see the light of the day [2].
Previously it was mainly inserted in postpartum, post abortion phase and as an interval contraception. Later WHO advocated insertion of Cu T in post placental phase following vaginal delivery and during cesarean sections. Multiple studies were done to find out the problems associated with the post placental insertion. Problems like refusal for insertion of device, spontaneous expulsion, request for removal of Cu T and missing threads were reported.
An IUCD is one of the safest one-time insertion methods of contraception, both for inter-pregnancy gap as well after completion of family. There is no doubt that Cu T helps in immediate contraception [7,8,9]; however, the caregivers should ensure that a mere insertion is not the end point of their services. Patients with misplaced IUCDs may present with pregnancies or ‘lost strings’ or they may remain asymptomatic; but the complications associated and mental stress for its removal outweighs in general population, especially when patient has to go through referrals at other centres and undergo a long and painful procedure for its removal; resulting in negative impact on the image of nearly an ideal contraceptive. It is therefore essential, that efforts should be directed to analyse complication rates that may be hampering its use. This may help rectify and boost confidence of health care providers to draw more couples towards contraceptive services.
With scant literature on the expulsion rate, missing thread and related complications at different time period of Cu T insertion, the present study was planned to study various aspects associated with missing thread of Cu T. The intention is better awareness of association of time of insertion and probability of expulsion, misplacements and difficulties in removal and to find probable solutions.
Materials and methods
After approval of the study by research and institutional Ethics Committee, for present study retrospective analysis of patients who underwent management for missing CuT thread in Minor Operation theatre on Outdoor patients (OPD) basis or as a major intervention in Major Operation theatre was carried out by collecting information from hospital records and duly completed with telephonic contact with such women. Study was further extended prospectively on patients referred from various institutes, detected missing thread while examination and reporting to have missing CuT threads. A written informed consent was obtained from subjects. All details were recorded on proformas. In addition, Data was analysed with various interrelated factors, namely, relation to timing of insertion, presentation, complications, number and kind of interventions for its removal. Literature search for possible suggestion on remedies was also made.
Inclusion criteria
• Patients reporting with inability to feel Cu T threads
• Incidental detection due to non-visualisation of Cu T threads
on examination
• Referred to us with the complaint of missing Cu T thread
• From minor or major OT records
Exclusion criteria
• Patients requiring Cu T removal with visible thread
Statistical analysis
The data was entered in excel sheet. Statistical analysis was done using SPSS software (statistical package for the social sciences), version 26. The proportion of women with missing Cu T thread were calculated among all women attending OPD and IPD by using percentages. Complication rates in different subgroups of patients were compared by using normal test of proportion. Correlation between different groups could not be calculated because of major difference in the number of subjects in the groups.
Results
In total 69 women consulted our OPD with the complaint of missing thread of CuT, of which 57 women could be contacted telephonically. Only 7 women had failed to feel the thread and reported for removal, for rest missing thread of CuT was diagnosed by doctor during physical examination. Amongst these 23 had been referred and 32 women had chosen to report to our institute on their own. In 2 women CuT was diagnosed as incidental finding.
Amongst these, 42 (60.87%) had Cu T removal in minor OT attached to our OPD, using long artery forceps, Cu T removing hook or uterine curette successfully. 21 (30.43%) women required hysteroscopy assisted removal, 2 (2.89%) women underwent laparotomy and amongst 4 (5.79%) Cu T was not localized suggesting spontaneous expulsion.
In 2 patients unaware of Cu T insertion, one presenting with pyometra, ultrasound examination revealed Cu T that was removed along with drainage of pyometra. In the other patient during hysterectomy for AUB-L, Cu T piercing in uterovesical fold was identified.
For 2 women the thread had coiled up and though could be seen, both opted for removal of CuT and for both unfortunately thread broke while removal. For purpose of this study both have been included amongst our subjects.
As for number of attempts for removal, for 25 women first attempt were successful for removal. 13 women each had one and more than 1 previous failed attempts. 2 women were directly taken up for hysteroscopic removal of Cu T.
19 women opted for reinsertion of the device wilfully on their own and 32 could be counselled and reassured for its reinsertion, 6 were not sure. Out of these women, 13 had used CuT even earlier, 2 had used barrier method and for 42 no contraception had been used earlier.
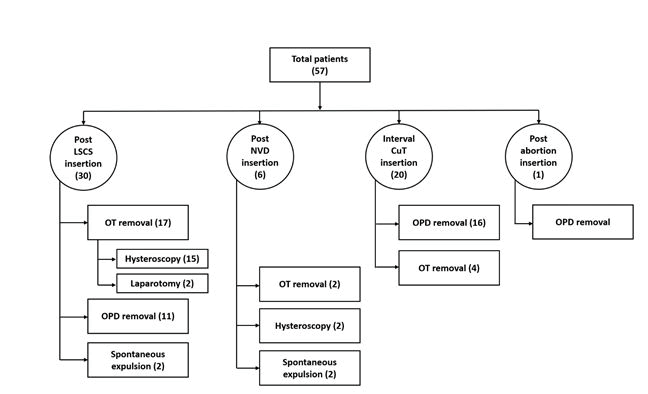
In reference to the timing of insertion for 30 women Cu T had insertions during LSCS and for 6 immediate post vaginal delivery, 20 had interval Cu T insertion, only one insertion followed post abortion. (Figure A1)
For all the women demanding or advocated CuT removal, a set sequence of management was evident. After history and examination, an attempt to remove CuT was made in the OPD for all women, who had USG report showing CuT insitu with the exception of two (who were directly taken up for hysteroscopic removal) and successful in 42 women. Rest women were planned for operative management accordingly.
On ultrasonography in 42 women, CuT was found in position, miss-positioned in 7, misplaced in 1 and not seen in 4. USG helped detect one forgotten CuT with pyometra and missed in 1 patient lying in utero-vesical fold, otherwise not even known to the patient. For 2 patients with coiled threads USG was not felt required before removal. (Table No. B1)
| USG findings | Patients number (n = 57) |
|---|---|
| Mid position | 42 |
| Mispositioned within uterus | 7 |
| Outside but alongside uterus | 1 |
| pyometra with Cu T | 1(not amongst 57) |
| Incidental detection | 1 |
| not seen | 4(spontaneous expulsions) |
| not done | 2 (coiled thread) |
Table1: USG findings.
USG- ultrasonography, CuT- copper T
There were total 8 patients in whom CuT was not in normal postion. In 7 women CuT was found to be inside the uterine cavity but malpositioned, like inverted, indenting the uterine fundus. In one-woman CuT was lying alongside external wall of the uterus which intra-operatively found to be coming out through fimbrial end of left fallopian tube. (Table No. B2)
| Misplaced / mispositioned Cu T | Number of patients |
|---|---|
| Total | 8 [100%] |
| Post LSCS | 4 [50%] |
| Post NVD | 3[37.5%] |
| Interval | 1 [12.5%] |
Table2: Misplaced / mispositioned Cu T finding on USG in reference to timing of insertion.
CuT- copper T, LSCS- lower segment cesarean section, NVD- normal vaginal delivery
It is pertinent to note that for 30 women for whom CuT was inserted during LSCS, Cu T could be removed in OPD only in 11 (36.67%) and 17 (56.67%) required operative intervention. For 15 it was feasible to remove it via hysteroscopy but for 2, laparotomy had to be resorted to. These included 4 (13.33%) women who had misplaced CuT. For 2 spontaneous expulsions was declared on the basis of non-localization of CuT on X-ray.
20 women got interval CuT insertion. Out of all these in 16 (80%) women, removal was done in OPD and 4(20%) women had to undergo hysteroscopic CuT removal.
We could find only 6 women who got CuT insertion immediately after vaginal delivery. Out of 6, 2 (33.3%) had CuT removal by hysteroscopy, 2 (33.3%) had spontaneous expulsion and 2 (33.3%) had CuT removal in OPD. (Table No. B3).
| Cu T insertion | Post NVD | Post LSCS | Interval insertion | Post abortion | |
|---|---|---|---|---|---|
| Total | 6 (100%) | 30 (100%) | 20(100%) | 1(100%) | |
|
OT removal |
|
2 (33.33%) |
17 (56.67%) |
4 (20%) |
0 |
|
|
Hysteroscopy |
2 (33.33%) |
15 (88.23%) |
4 (100%) |
0 |
|
|
Laparotomy |
0 |
2 (11.76%) |
0 |
0 |
|
OPD removal |
|
2 (33.33%) |
11 (36.67%) |
16 (80%) |
1 (100%) |
|
Not tracable |
Spontaneous expulsion |
2 (33.33%) |
2 (6.66%) |
0 |
0 |
|
Mispositioned/misplaced |
|
3 (50%) |
4 (13.33%) |
1 (5%) |
0 |
Table3: Cu T removal in relation to post NVD/ post LSCS/ interval and post abortion insertion.
CuT- copper T, LSCS- lower segment cesarean section, NVD- normal vaginal delivery, OT- operation theatre, OPD- out patient department
Discussion
Worldwide, over 128 million women rely on intrauterine contraceptive devices (IUCD) for contraception, making it as one of the most commonly used reversible method of contraception among married women of reproductive age. They are of two types of IUCD’s, hormonal and non-hormonal. CuT is non-hormonal IUCD and is provided free of cost by Government of India. It provides very effective, safe and long-term protection against pregnancy, with prompt return to fertility upon removal. Their use is convenient, don’t interfere with sexual activity, do not require daily action on the part of the user or repeated clinic visits for supplies and provide long term contraceptive effect even if patient avoids follow up. IUCDs have limited contraindications like acute pelvic infections, uterine malformations and known case of carcinoma cervix. It has a failure rate of less than 1%. It can be inserted either as an interval procedure or after abortion or delivery. All IUCDs have threads which help in removal of the device, reassures its correct placement and retention. In cases where thread is not visible, most of the times IUCD can be removed by IUCD removing hook (commonly known as copper removal hook) as an OPD procedure.
In India only 2% of married women of reproductive age use IUCDs. Soon after the delivery female and her husband are usually most motivated for interval and so for the contraception. Considering these facts Government of India promotes CuT insertion soon after the delivery. But despite the fact that the Government of India offers IUCD services free of cost, it still remains largely underutilized.
Cu T is a non-hormonal IUCD, with few selective problems like device expulsion, missing threads at follow-up and the tendency of increased puerperal bleeding. Missing thread being a significant problem specifically for setups where ultrasound is not available is concerning. Yet there is scarcity of literature on the issue and needs more attention.
One such study suggested, change in design of the device or application of a suture to ensure visibility of strings and adjustment and to ensure cost effective hormone releasing devices to reduce puerperal bleeding [3].
Another study on 324 IUCD users reported 21.29% (69) subjects with missing IUCD threads. Of these about half were asymptomatic and AUB being the commonest symptoms in others. Of these USG confirmed IUCD in situ (82.6%) Displacement was seen in 10.14% & embedment in 4.35%. Expulsion was quoted in 4.35% women. Removal was done in only 29 women. In 24 women CuT was removed in OPD, as minor OT procedure in 3 and only 1 required removal via hysteroscopy procedure. Commonest cause of missing threads was reported to be broken, detached or severed strings [4].
Contrarily for removal of IUCD with missing threads amongst 37 patients, 12 (32.4%) were removed by simple curettage or using IUCD hook under ultrasound guidance, 21 (56.7%) were removed under hysteroscopy guidance, 1 (2.7%) required laparoscopy and 3 (8.1%) required laparotomy. Noticeably in this study most of post placental insertion of IUCD s were found to be embedded into uterine myometrium or perforated the uterus and required either endoscopy or laparotomy for removal [5].
While in a study only reporting on Hysteroscopy assisted removal in 32 such cases, quoted IUDs easy removed by withdrawal holding vertical limb with no major immediate or late complication. Post procedure pain was complained by few women who needed intravenous sedation in addition to the paracervical block [6].
The present study was planned to evaluate the co-relation of this complication with special reference to time of insertion of Cu T and intervention required for removal of thus placed IUCD.
The study reveals definite impact timing of CuT insertion on incidence of misplacement and expulsion. The is understandable for involution of uterus and lax cervical opening for intrapartum or immediate post-partum insertions. This also justifies the increased failure of removals attempted as OPD procedure. Whether blind procedures increase misplacement is difficult to predict but immediate referral to a higher centre would avoid deeper imbedding. The exact incidence of CuT being removed is not known and it is possible with little skilful manipulations many mis-positioned CuT must be even getting removed in many hospitals. Contrarily even in tertiary level institutes need for surgical intervention was felt.
From aspect of safety hysteroscopy is ideal specifically after an attempt of failure of removal by Cut Hook. There can be a personal choice as in our unit for multiple attempts outside, not to woman to blind procedure, which is otherwise a choice under USG guidance as our first attempt for centrally placed CuT. CuT hook or a long artery are equally preferred instrument for low placed CuT but for one misplaced higher up hysteroscopy is ideal. Using a curettage can be anticipated to be damaging to endometrial lining and may be associated even with a risk of deepening misplaced Cut further.
One of the causes for missing threads could be expulsion with even missed by the user. In an attempt to highlight this problem a study suggested improvisation of device design or application of a suture technique to ensure strings visibility, adjustment and eventually to reduce chances of expulsion. Prevention of misplacement may prove beneficial in reducing puerperal bleeding also [3]. Since hormone releasing devices reduce even bleeding availability of cost-effective hormone releasing would be a double boon as reversible contraceptive in addition to correction of anaemia in developing countries.
From the results of our study, we suggest that common Information Performa should be developed for all Cut insertions at all centres so that more data can be analysed, to anticipate which patients are at a greater risk of misplacements and expulsions and need early referral to tertiary centres and so that SOP’s [standard operating procedures] can be developed for their follow ups. This will help in streamlining the management of such cases and hence will avoid the troubles faced by patients.
Conclusion
Our study concluded that there is definite impact of timing of CuT insertion on incidence of misplacement and expulsion. Immediate referral should be done to avoid deeper imbedding and blind procedures should be avoided. USG guided removal should be the first attempt for CuT removal whereas Hysteroscopy is ideal in cases of failed removal by CuT hook. More studies and data needed for developing a common information performa to develop SOPs for follow up of such patients.
References
- Johri V, Vyas KC. Misplaced Intrauterine Contraceptive Devices: Common Errors; Uncommon Complications. J Clin Diagn Res. 2013; 7(5): 905-907.
- Annual report of department of health and family welfare: Ministry of health and family welfare;2017-2018.
- Nelson AL, Massoudi N. New developments in intrauterine device use: focus on the US. Open Access J Contracept. 2016; 7: 127–141.
- Verma U, Gupta M, Saini V. Missing IUCD strings: an analysis. Int J Reprod Contracept Obstet Gynecol. 2018; 7(10): 4061-4067.
- Vasanthalakshmi GN, Subasri, Priyadarshini K. Management of missing threads of IUCD. Indian J Obstet Gynecol Res. 2017; 4(4): 416-419.
- Trivedi SS, Goel M, Jain S. Hysteroscopic management of intrauterine devices with lost strings. Br J Fam Plann. 2000; 26(4): 229-230.
- Jain R, Bindal J. Evaluation of Post-Placental and Intra-Cesarean Insertion of Copper-T 380A as a Method of Contraception. J Med Sci Clin Res. 2018; 6(6): 871-7.
- Dewan R, Dewan A, Singal S, Bharti R, Kaim M. Non-visualisation of strings after postplacental insertion of Copper-T 380A intrauterine device. Fam Plann Reprod Health Care 2017; 43: 186–94.
- Malik J, Das A, Rai P, Das S. Post placental copper-T 380A insertion after normal vaginal delivery and cesarean section and its clinical outcome. Int J Reprod Contracept Obstet Gynecol. 2016; 5(7): 2254-6.
- Ranjana, Verma A, Chawla I. A follow up study of postpartum intrauterine device insertion in a tertiary health care centre. Int J Reprod Contracept Obstet Gynecol. 2017; 6(7): 2800-5.
- Singal S, Bharti R, Dewan R, Divya, Dabral A, Batra A et al. Clinical Outcome of Postplacental Copper T 380A Insertion in Women Delivering by Caesarean Section. J Clin Diagn Res. 2014. 8(9): 1-4.
- Cremer M, Bullard KA, Mosley RM, Weiselberg C, Molaei M, Lerner V et al. Immediate vs. delayed post-abortal copper T 380A IUD insertion in cases over 12 weeks of gestation. Contraception. 2011. 83; 522–527.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences