Postpartum Family Planning Utilization and Associated Factors among Women Who Gave Birth in the Past 12 Months, Hawassa Town, Southern Ethiopia: A Community Based Cross-Sectional Study
Kebede Tefera* and Mulugeta Abuye
Published Date: 2023-05-05DOI10.36648/2471-9749.8.1.002
Kebede Tefera1* and Mulugeta Abuye2
1Department of Medicinal and Health Sciences, Hawassa University, Hawassa, Ethiopia
2Department of Medicinal and Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- *Corresponding Author:
- Kebede Tefera Department of Medicinal and Health Sciences, Hawassa University, Hawassa, Ethiopia, Tel: 911975936; Email: ktefera2015@gmail.com
Received: October 25, 2019, Manuscript No. IPJCS-23-2807; Editor assigned: October 30, 2019, PreQC No. IPJCS-23-2807 (PQ); Reviewed: November 13, 2019, QC No. IPJCS-23-2807; Revised: April 05, 2023, Manuscript No. IPJCS-23-2807 (R); Published: May 05, 2023, DOI: 10.36648/2471-9749.8.1.002
Citation: Tefera K, Abuye M (2023) Postpartum Family Planning Utilization and Associated Factors among Women Who Gave Birth in the Past 12 months, Hawassa Town, Southern Ethiopia: A Community Based Cross-Sectional Study. J Reproduct Health Contracept Vol: 8 No: 1:002.
Abstract
Background: Addressing family planning in the postpartum period is crucial for better maternal, neonatal and child survival because tenable women to achieve healthy interval between births. Many women do not realize that they are at a risk for pregnancy during this period. Thus, the objective of this study was to assess the utilization of postpartum family planning services among postpartum women and associated factors in Hawassa, Ethiopia.
Methods: A community based cross-sectional study was conducted among 381 women in Hawassa city from April to May 2018 in Hawassa city. Study subjects were selected by systematic random sampling technique. Structured questionnaire was used to collect the data through interview. Data analyzed by SPSS 20. Multi-variable logistic regression was used and significance declared at p-value ≤ 0.05.
Results: The prevalence of contraceptive utilization was found to be 147 (38.6%) among women in the postpartum period. The majority of current contraceptive users were injectable (35.4%). The odds of postpartum family planning utilization was statistically significantly associated with received FP education after delivery at immunization service (AOR=4.11; 95% CI; 2.143, 7.864), mothers’ discussion with husband on family planning issue (AOR=9.7; 95% CI; 4.15, 22.6), Family planning problem (AOR=0.5; 95% CI; 0.28, 0.89), 0-6 month of postnatal period (AOR=0.23; 95% CI; 0.124, 0.430) and 1-4 number of pregnancy (AOR=0.05; 95% CI; 0.0124, 0.170), History of abortion (AOR=0.23; 95% CI; 0.124, 0.430).
Conclusion: Postpartum family planning use is still low. Consequently, this finding implies the need to get better with those factors to enhance the uptake of postpartum modern contraceptive through well-organized family planning education and follow up for the reproductive age women.
Keywords
Postnatal care; Family planning utilization; Postpartum; Reproductive; Abortion
Introduction
Back ground
Family planning allows individuals and couples to anticipate and attain their desired number of children by the spacing and timing of their births. Addressing family planning in the postpartum period is paramount for better maternal, neonatal and child survival because it enables women to achieve healthy interval between births. In the first year after women have given birth, do not realize that they are at risk of pregnancy. Consequently, contraceptive use by women during this period is low resulting to unintended pregnancies and unwanted childbearing/low utilization of postpartum family planning services. Unmet need for family planning is extremely high particularly among women in the postpartum period. More than 90% of postpartum women in developing countries desire to space or limit a subsequent pregnancy, yet 61% are not using a family planning method. This means that service providers are not getting postpartum women for the family planning options that they want. Only a minority of these women uses a family planning method, and many do not use the modern contraceptive methods consistently between a birth and next pregnancy [1].
Though most women want to delay their pregnancy for at least two years after giving birth, postpartum family planning/ PPFP use is low. Uptake of PPFP has the potential to make a large contribution toward the global goals, yet it remains unavailable to millions of women and girls in the developing world. PPFP is a service delivery strategy that expands access to FP through integration within the existing continuum of maternal, newborn and child health services. Wellimplemented, national PPFP programs that deliver family planning services to postpartum women in the first two years after birth using these integrated channels are an essential platform for reaching global FP goals and saving lives of women and children at the same time. Now is a better time than ever to increase access to this life-saving intervention. With updated guidance from the world health organization, more postpartum contraceptive options are available than ever before. More women across the globe want to plan their families. More countries are including PPFP in their health strategies. Recognizing this opportune time, global health leaders have stimulated a worldwide movement around greater access to PPFP [2].
Family planning enhances efforts to improve family health. However traditional beliefs, religious barriers, misconceptions, lack of male involvement and the likes weakened family planning interventions. Nowadays, the commitment of governments both at national and international levels to avail a wide range of family planning choices to their communities is indeed boosting. Despite this promising condition, the unmet need for family planning is extremely high particularly among women in the postpartum period. Postpartum family planning as part of a comprehensive MNCH approach has the potential to systematically reach a large number of women with critical, lifesaving information and services. The first year after a woman has given birth is crucial period for uptake of contraceptives to prevent unintended pregnancy. However, many women do not realize that they are at risk for pregnancy during this period. Hence, the first year after birth is given less emphasis regarding contraceptive utilization and the contraceptive use by women during this period is low .In line with Ethiopia’s Family Planning (FP2020) commitments, the Federal Ministry of Health (FMoH) developed the health sector transformation plan of 2015, which aimed to increase the Contraceptive Prevalence Rate (CPR) to 55% by 2020. To achieve this and other related global and national targets, the uptake of Postpartum Family Planning (PPFP) has the potential to make a large contribution and it should be supported by different scientific evidences to maximize its utilization and the intended benefit of the community [3].
EDHS 2016 report shows that the Contraceptive Prevalence Rate (CPR) for currently married women age 15-49 is 36%, with 35% using modern methods and 1% using traditional methods [4]. Though this report shows that there is a significant increase of modern family planning utilization from time to time, there is still a substantial difference between what it is and what it should be; and the reasons for this difference needs further assessment; Hence, this study assessed the utilization of postpartum family planning services and associated factors among women who gave birth in the past twelve months prior to the interview of the study. In general, globally the benefits of family planning for both maternal and infant health have well documented, about 25% to 40% of maternal death could be averted if unplanned and unwanted pregnancies were prevented [5].
About 10% of reduction in child death can be achieved (one million under five deaths averted annually by eliminating interbirth interval of less than two years). Despite this accumulation of evidence the current status of postpartum family planning utilization is still poor, postpartum FP provision is relatively straight forward service, yet it has not been systematically addressed by either maternal, neonatal or child health/family planning program. Ethiopia is one of the most populous countries in Africa next to Nigeria, which suffers from direct and indirect population problems. Uncontrolled fertility has adversely influenced the socio-economic, demographic and environmental development of the country. The demographic significance of Ethiopia population growth on the Africa continent is substantial [6].
According to the Ethiopian house and population census in 2007 the country’s population growth rate is 2.6%. EDHS 2016 report indicates that total fertility for the 3 years preceding the survey is 4.6 children per woman (2.3 in urban areas and 5.2 in rural areas) nationally and 4.4% in SNNPR. The proportion of women age 15-49 in Ethiopia who received ANC from a skilled provider has increased from 27% in 2000 to 34% in 2011, and 62% in 2016. 32% of women had at least four ANC visits during their last pregnancy. For the 5-year period preceding the survey, the under 5 mortality rate is 67 deaths per 1,000 live births, and the infant mortality rate is 48 deaths per 1,000 live births. Evidences have shown that encouraging early ANC visits, institutional deliveries, postnatal care, and contraceptive adoption are the key elements in improving safe motherhood. As the first pillar of safe motherhood and essential component of primary health care, contraceptive plays a key role in reducing maternal and newborn morbidity and mortality by preventing unintended pregnancy and close birth intervals [7].
SNNPR has the fertility rate of about 4.4 children per woman, while Addis Ababa has a below-replacement level of fertility of 1.8 children per woman. As a result of the low contraceptive prevalence, many women of reproductive age who want to stop or postpone low child bearing are not able to do so; and hence there is a high unmet need for contraception in SNNPR, estimated at 22% in 2016. Therefore, this study was carried out to assess the utilization and associated factors for postpartum family planning services among women who gave birth in the past 12 months in Hawassa city, SNNPR; Ethiopia in 2018. It generates evidence-based information which enhances the local health planner and stakeholders working on the programs of family planning services with the aforementioned benefits and intern provide a contribution for attaining Sustainable Development Goal (SDG) which aimed to improve family planning services [8].
Materials and Methods
Study setting and period
This study was conducted in Hawassa city from April 25, 2018 to May among women who gave birth in the past 12 months, Hawassa study area. Hawassa is located 273 km south of Addis Ababa, the capital of Ethiopia. The city serves as the capital of the Southern Nations, Nationalities, and Peoples' Region (SNNPR) [9].
There are 6 hospitals, 6 health HCs, 52 clinics, 14 pharmacies and 152 other health facilities owned by government and non- government organizations giving services to Hawassa and nearby residents. The city administration is structured by 8 sub cities and 32 kebeles (the lowest administrative structure). Based on 2015 population projection by the Central Statistical Agency (CSA), the Hawassa city administration has a total population of 371,826, consisting of 191,352 males and 180,474 females. 87,751 (23.6%) the total urban population are women at reproductive age (15 yrs-49 yrs) and the number of estimated birth from the urban population per annual is about 13,014 (3.5%) [10].
Currently, a total of 120 urban health extension professionals are implementing Ethiopian urban health extension program at community level. On average, each of them expected to reach 500 households in their home-to-home services. Their services focus on maternal and other health services including follow up services at household level during their home-to-home visit. They have standard pregnant women and under1 children registrations to facilitate their follow up activities in their catchment. So, this study was benefit the use of these registrations with the lists of pregnant women to identify the postpartum women who gave birth in the past twelve months prior to the interview of the study in randomly selected kebeles (the smallest unit of administration) of the city for the purpose of the study. This somewhat simplified the sampling and data collection process as the health extension workers know the address and date of delivery of each postpartum woman in their respective catchment areas [11].
Study design
A community based cross-sectional study design was conducted.
Source and study population
The source population comprises all reproductive age women who give birth in the last 12 months prior to the study period in Hawassa city, SNNPR [12]. The study population was all women aged 15 to 49 years who delivered a baby in last 12 months duration prior to the study period from randomly selected kebeles (the smallest unit of administration) of Hawassa city [13].
Inclusion and exclusion criteria
Inclusion: Postpartum women who had given birth in the past 12 months and live in Hawassa city during data collection period, regardless of parity, religion, culture, education and maternal age included in the study [14].
Exclusion: The study excluded women who had experienced neonatal deaths after their current delivery.
Sample size determination
In Hawassa city the number of estimated birth per annual is about 13,014 (3.5%). As this study focuses on all reproductiveage women who gave birth in past 12 months prior to the study period, the total number of target population for this specific study is N=13,014. Accordingly, sample size was calculated using the single population proportion formula n=(Zα/2)2 P(1-P)/(d2) considering the 63% prevalence of postpartum modern contraceptive knowledge in Hawassa city, Ethiopia, the use of a 95% Confidence Interval (CI) and a 5% margin of error (d). After considering the 10% non-response rate, the total sample size is calculated to be 394 [15].
Sampling procedure
First of all, five kebeles (the smallest unit of administration) were selected purposely out of 32 kebeles of Hawassa city. The number of estimated birth in each of the selected kebele per annual is 310, 359, 144, 245 and 229 respectively. To get a total of 394 postpartum women from these kebeles, allocated the sample size proportionally. Then principal investigator had got a list of postpartum women from each kebele and randomly selected a proportional number of postpartum women from each of the selected kebeles by deploying systematic sampling method. The first postpartum woman was selected by lottery method. The postpartum women who had experienced neonatal death after their most recent delivery were excluded and replaced by another one in the list. The selected postpartum women interviewed using pre-prepared questionnaire and their responses were recorded by trained data collectors.
Data collection procedures and tools
Interviewer-administered questionnaire was used to collect data using face to face interview by the trained five data collectors prior to the data collection exercise and they monitored and assisted by the principal investigator. To avoid conflict of interest and to collect data free from bias, the data collectors were not health professionals. Besides, to ensure reliability and validity of the data collection instrument, pretesting is done on 18 postpartum mothers (5% of total sample size) at other adjacent kebeles (the smallest unit of administration) within the city. The components of the questionnaire were demographic data, knowledge of mothers about PPFP services, beliefs related to PPFP services, influence of social networks and past experience related to FP method use.
Operational definition
Extended postpartum period: The 12 months period after a live birth.
Utilization of postpartum modern contraceptive: When a postpartum woman reported actively using any modern contraception methods (pill, intrauterine device, injectable, condom (men or women), sterilization (men or women), or implants) during the 12-month following her most recent childbirth [13].
Knowledge of modern contraception methods: When a woman mentioned at least one modern contraceptive method, she was considered knowledgeable.
Attitude for modern contraception methods: A postpartum woman has a favorable attitude for PPFP utilization if the sum of her respond for agrees and strongly agrees is more than 3 of the 6 questions (more than 50%) which are related to the postpartum women’s attitudes for PPFP utilization.
Data quality management
Data quality is controlled through the provision of training to the data collectors about the overall data collection procedures and the techniques of interviewing. A pre-test done using 5% of the sample questionnaire before the actual data collection in other kebeles of the city, to ensure the clarity of the questionnaire, to check the wording, and to confirm the logical sequence of the questions with a population of postpartum women assumed to have similar socio-demographic characteristics to the population of the study area, and necessary corrections were made based on the pre-test findings. The collected data was checked for completeness, consistency, accuracy and clarity by the principal investigator on a daily basis. Finally, the completeness of the questionnaire was checked before entering data into the computer software program and before analysis and interpretation.
Data management and analysis
The data were entered and cleaned using Epi data version 3.1, then exported to and analyzed with SPSS version 20. For the descriptive analysis, continuous variables were summarized using means, and Standard Deviations (SDs), while categorical variables were summarized using proportions. Both bivariate and multivariate logistic regressions were used to identify factors associated with postpartum modern contraceptive use. Variables with a p-value<0.25 in the bivariate analysis were fitted into a multiple logistic regression model to control for confounding effects. Adjusted Odds Ratios (AOR) with 95% CIs were used to identify factors associated with postpartum modern contraceptive use. The p-values <0.05 were considered to indicate statistically significant of the associations with postpartum modern contraceptive use. Finally, results were compiled and presented using tables, graphs, and texts.
Results
Socio-demographic characteristics of the study participants
Among 394 study participants, 381 postpartum women were interviewed, resulting in 97% response rate. The mean (± SD) age of the respondent was 30.31 ± 4.19 years and ranging from 21 to 41 years. The majority of the respondents, 374 (98%) were married. Of the total respondents, majority were orthodox 177 (46.5%) in the religion. Concerning educational status 165 (43.3%) of the postpartum women have attended secondary school (Table 1).
| Variables | Frequency | % (%) |
|---|---|---|
| Age category | ||
| 20-24 year | 23 | 6 |
| 25-29 year | 150 | 39.4 |
| 30-34 year | 139 | 36.5 |
| 35-39 year | 60 | 15.7 |
| 40-44 year | 9 | 2.4 |
| Marital status | ||
| Married | 360 | 94.5 |
| Others (Single, Divorced) | 21 | 5.5 |
| Religion of respondent | ||
| Orthodox | 177 | 46.5 |
| Muslim | 40 | 10.5 |
| Protestant | 149 | 39.1 |
| Catholic | 15 | 3.9 |
| Educational level of respondents | ||
| Illiterate | 7 | 1.8 |
| Literate (primary and above) | 371 | 98.2 |
Table 1: Socio-demographic characteristics of women in the postpartum period in Hawassa city, South Ethiopia, May 2018 (n=381).
Reproductive and reproductive health servicerelated characteristics
Almost half of the respondents were experienced 1-4 pregnancies 339 (89%). The mean number of living children was 2.27 per women (SD, ± 1.03). Two hundred forty two (63.5%) of the respondents were stated that they have 1-2 living children. Majority of respondents were never experienced miscarriages or abortions 294 (77.2%). Two hundred thirty two (61%) of the respondents were with 0-6 months of postpartum period .About 132 (34.6%) respondents wanted to have another child within the next 2 yrs. The majority of the women 295 (77.8%) discussed with their spouses about the number of children they planned to have as a couple and 90.5% (133) of current PPFP users are the respondents who were discussed with their husbands. Two hundred fifty five (66.9%) respondents wanted to have 4-5 children and about 59 (15.5%) wanted more than 6 children in their life.
Three hundred forty three (90%) of the study participant had ANC visits at least once. It was only 95 (27.7%) had attend the recommended four and more ANC visits. More than half, 210 (55.1%) of the respondents were received counseling about FP services before delivery at Antenatal clinic and also a ter delivery, 164 (43%) of respondents reported that they received counseling of FP services at the time of home to home visits of health providers (urban health extension workers) (Table 2).
| Variables | Frequency (381) | % (%) |
|---|---|---|
| No. of pregnancies | ||
| 1-4 | 339 | 89 |
| >4 | 42 | 11 |
| No. of living child | ||
| 1-2 | 242 | 63.5 |
| 3-4 | 137 | 36 |
| >4 | 2 | 0.5 |
| No. of miscarriages or abortions | ||
| Not at all | 294 | 77.2 |
| Yes | 87 | 22.8 |
| Period of PP/Age of last child | ||
| 0-6 months | 232 | 61 |
| 7-12 months | 149 | 39 |
| When do you intend to have another child | ||
| 2 years | 132 | 34.6 |
| 3 years | 138 | 36.2 |
| ≥ 4 years | 64 | 16.8 |
| I don’t know | 47 | 12.3 |
| How many children do you intend to have in life | ||
| 2-3 children | 67 | 17.6 |
| 4-5 children | 255 | 66.9 |
| 6-8 children | 59 | 15.5 |
| Did you attend antenatal clinic during pregnancy | ||
| Yes | 343 | 90 |
| No | 38 | 10 |
| How many times did you attend the antenatal clinic | ||
| One visit | 14 | 4.1 |
| Two visit | 90 | 26.2 |
| Three visit | 144 | 42 |
| Four and more visit | 95 | 27.7 |
| Where was the place of delivery for your last child | ||
| Health facility | 380 | 99.7 |
| Home | 1 | 0.3 |
| Type of facility of delivery (n=380) | ||
| Public health facility | 274 | 72.1 |
| Private health facility | 106 | 27.9 |
| Did you get postnatal service after delivery | ||
| Yes | 300 | 78.7 |
| No | 81 | 21.3 |
| Where received education about FP services before delivery of last child | ||
| Antenatal clinic | 210 | 55.1 |
| Family planning clinic | 21 | 5.5 |
| During home visits by providers | 150 | 39.4 |
| Where received education about FP services after delivery of last child | ||
| Postnatal ward | 65 | 17.1 |
| EPI visit | 152 | 39.9 |
| During home visits by providers | 164 | 43 |
| Ever discussed with husband number of children do you intend to have in life | ||
| Yes | 295 | 77.4 |
| No | 86 | 22.6 |
| Did you experience any problem with the methods | ||
| Yes | 169 | 44.4 |
| No | 212 | 55.6 |
| Currently use of contraception method | ||
| Yes | 147 | 38.6 |
| No | 234 | 61.4 |
| Ever discussed with husband FP use (n=147) | ||
| Yes | 133 | 90.5 |
| No | 14 | 9.5 |
Table 2: Reproductive and reproductive health service-related history of postpartum mother at Hawassa city, South Ethiopia, May 2018 (n=381).
Knowledge of the participants about contraceptive method
From the total respondents 381 (100%) had awareness of modern family planning among postpartum women. Regarding the general uses of contraceptive, one hundred thirty one (41.6%) of the respondents had awareness of contraceptive method that it prevents unwanted pregnancy (Table 3).
| Variables | Frequency | % (%) |
|---|---|---|
| Awareness of family planning methods (Do you know different types of modern contraceptive methods) | ||
| Yes | 381 | 100 |
| No | 0 | 0 |
| What are the general uses of contraceptive do you know | ||
| Help for prevention of unwanted | 148 | 38.8 |
| Prevention of possible maternal | 14 | 3.7 |
| Limiting number of children | 84 | 22 |
| Child spacing | 70 | 18.4 |
| all of the above | 65 | 17.1 |
Table3: Knowledge of family planning among postpartum women in Hawassa city, South Ethiopia, May 2018 (n=381).
Attitude of postpartum women towards contraceptive methods
About 301 (79%) of respondents cited that reason behind utilization of modern contraceptive methods as FP helps mothers to regain their strength before their next baby by strongly agreeing it. Sharing responsibility of FP use with men is the next factor that mothers strongly agreed with for using the contraceptive methods 221 (58%) of the respondents. About 282 (74%) of respondents reported that their husbands decide if wife wants to use contraceptive while 91 (24%) said that their husbands are not responsible person to decide use of contraceptive methods. Majority of the respondents 362 (95%) believe that child spacing protects mother and child death and only 53 (14%) of participants reported that FP methods has side effects; it will be dangerous to a mother (Table 4).
| Attitude statements | Strongly agree (%) | Agree (%) | Disagree (%) | Strongly disagree (%) | Indifference (%) |
|---|---|---|---|---|---|
| Husband decides if wife wants to use | 44.60% | 29.10% | 19% | 5.50% | 1.80% |
| Child spacing protects mother and child death | 52% | 43% | 5% | 0% | 0% |
| FP methods has side effects; it will be dangerous to a mother | 0.50% | 13.10% | 81.60% | 4.70% | 0% |
| FP practice will cause a loss of confidence between couples | 2% | 10% | 51% | 35% | 2% |
| Men should share the responsibility of FP use | 58% | 29% | 7% | 2% | 3% |
| FP helps a mother to regain her strength before her next baby | 79% | 12% | 6% | 2% | 1% |
Table 4: Attitude statements of study participant about contraceptive methods, Hawassa, South Ethiopia, May 2018 (n=381).
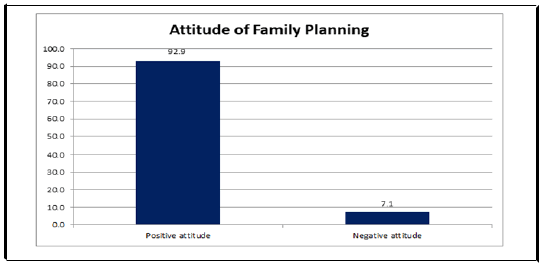
Among 381 those who had awareness family planning methods revealed that 354 (92.9%) of the study participants were positive attitude for FP utilization and among 147 PPFP users about 138 (94%) of the respondents had favorable attitude for PPFP utilization (Figure 1).
Current delivery of postpartum family planning utilization
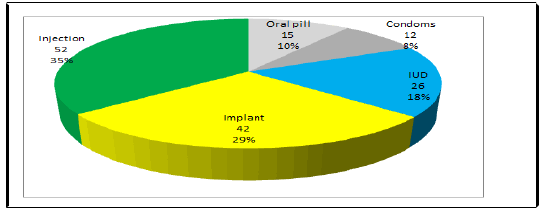
One hundred forty seven (38.6%) of the respondents reported that they were using contraception following their current delivery. About 166 (70.9%) of the respondents mentioned that the reason behind not using contraception was as they perceived they were not at risk of pregnancy in the period (Table 5). Among 147, majority 52 (35.4%) of the respondents was preferred to use injectable contraceptive followed by Implants 42 (29%) (Figure 2).
| Variables | Frequency | % (%) |
|---|---|---|
| Are you currently using any method of contraception (n=381) | ||
| Yes | 147 | 38.6 |
| No | 234 | 61.4 |
| If no why (n=234) | ||
| Delivered recently | 43 | 18.4 |
| Having another child | 14 | 6 |
| Not married | 4 | 1.7 |
| Religious restrictions | 3 | 1.3 |
| Feel not at risk of pregnancy | 166 | 70.9 |
| Others | 4 | 1.7 |
Table 5: Current postpartum FP utilization of study participants, Hawassa city, South Ethiopian, May 2018.
Factors associated with postpartum contracept ve use
All the variables that possess significance in the bivariate analysis were included in a multivariable logistic regression analysis model. In the multivariate logistic regression analysis, the following variables were identified as independently associated with postpartum contraceptive use. These were: Problem with family planning method, number of pregnancy, Ever discussed with husband about FP, place where received FP education before and after delivery and history of abortion. Mother with discussion on family planning issue with husband had 9.7 times (AOR=9.7 95% CI: (4.15, 22.6)) higher odds of utilization of postpartum FP compared to those mothers with not discussed with their husbands higher odds of utilization of postpartum FP compared to those mothers with not discussed with their husbands. The variables where received FP counseling after delivery at immunization service and post natal ward had 4.11 times (AOR of 4.105; 95% CI: (2.143, 7.864)) and 3.96 times (AOR of 3.96; 95% CI: (1.906, 8.206)) respectively higher odds of utilization of postpartum FP compared to those mothers who received FP counseling a ter delivery at home visit by health providers. Mothers who had the experience any problem with family planning methods were 60% less likely to utilize postpartum FP compared to mothers with nonexperience any problem with family planning method (AOR of 0.4; 95% CI: (0.253, 0.604)).
Mothers who had experience of abortion were 86.8% less likely to utilize postpartum FP compared to mothers with nonexperience of abortion (AOR of 0.132; 95% CI: (0.05, 0.370)). Moreover, Postpartum mothers with one up to four history of pregnancy as had 95% less likely to utilize the postpartum FP compared to respondents with more than four history of pregnancy (AOR of 0.5; 95% CI: (0.05, 0.169)). Respondents with Postpartum period up to 6 months had less likely to utilize the postpartum FP compared to those mothers with last child greater than or equal to seven months (AOR of 0.23; 95% CI: (0.124, 0.426)) (Table 6).
| Variable | Current use of PPFP | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|
| yes (147) | No (234) | ||||
| No of pregnancy | |||||
| 1 up to 4 | 122 | 217 | 0.382 (0.199, 0.736) | 0.05 (0.012, 0.169) | <0.001 |
| >4 | 25 | 17 | 1 | 1 | |
| Period of postnatal (month) | |||||
| 0-6 | 75 | 157 | 0.511 (0.335, 0.780) | 0.230 (0.124, 0.426) | <0.001 |
| 7-12 | 72 | 77 | 1 | 1 | |
| Ever discussed with husband | |||||
| Yes | 133 | 162 | 4.222 (2.279, 7.823) | 9.7 (4.150, 22.6) | <0.001 |
| No | 14 | 72 | 1 | 1 | |
| Place where received FP counselling before delivery | |||||
| Antenatal clinic | 64 | 145 | 0.543 (0.351, 0.840) | 0.510 (0.258, 1.009) | 0.053 |
| Family planning clinic | 16 | 5 | 3.964 (1.381, 11.379) | 1.040 (0.309, 3.502) | 0.95 |
| During home visits by providers | 67 | 83 | 1 | 1 | |
| Place where received FP counselling after delivery | |||||
| Postnatal ward | 33 | 32 | 2.727 (1.504, 4.945) | 3.955 (1.906, 8.206) | <0.001 |
| EPI service | 69 | 83 | 2.198 (1.376, 3.513) | 4.105 (2.143, 7.864) | <0.001 |
| During home visit | 45 | 119 | 1 | 1 | |
| Experience any problem with modern family planning methods utilizations | |||||
| Yes | 45 | 124 | 0.391 (0.253, 0.604) | 0.497 (0.279, 0.885) | 0.018 |
| No | 102 | 110 | 1 | 1 | |
| Experience of abortion | |||||
| Yes | 29 | 58 | 0.746 (0.451, 1.233) | 0.132 (0.048, 0.365) | <0.001 |
| No | 118 | 176 | 1 | 1 | |
| Did you get postnatal service after delivery | |||||
| Yes | 124 | 176 | 1.777 (1.041, 3.033) | 1.614 (0.687, 3.79) | 0.272 |
| No | 23 | 58 | 1 | 1 | |
Table 6: Bivariate and multivariable logistic regression analysis of factors associated with utilization of postpartum family planning at Hawassa city, South Ethiopia, May 2018 (n=381).
Discussion
This study has investigated the magnitude and correlates of postpartum family planning utilization among all reproductive age women, who gave birth in the last 12 months prior to this study. In our study 38.6% of postpartum women were in use of contraceptives.
This finding is also consistent with a recent finding of Ethiopia Demographic and Health Survey 2016 that the Contraceptive Prevalence Rate (CPR) for currently married women age 15-49 is 36%, with 35% using modern methods and 1% using traditional method. However, this finding is less as compared to studies done in Nigeria (44%) and India (49%); and it is also lower than the prevalence of postpartum contraceptive in Jimma Mana district town 48.4%. But, it is by far higher as compared to study done at Kebribeyah town (12.3%) in Somali region, Eastern Ethiopia. This may be due to the temporal differences in the methodologies and/or the fact that there may be socio demographic, cultural, awareness, study time and religious difference for the uptake of postpartum family planning use.
Injectable (35.4%) and implant (29%) were the commonly used methods. Moreover, IUD and oral pills accounted for 18% and 10% of the users respectively. The degree of injectable preference was in line with study conducted in Gondar town. This might be attributed to client’s preferences for specific methods as well as the accessibility and availability of chosen methods. Women in the postpartum whose duration of postpartum from 7-12 months were more likely utilize postpartum contraceptive than duration less or equal to 6 months postpartum. This study was supported by crosssectional study conducted in Gonder town. This might be due to the duration of postpartum period increases women involved in sexual activity. Discussions with husband on contraception were significantly associated with the use of modern contraceptives in the postpartum period. Similar findings were reported in studies conducted in Ethiopia and in Nigeria. This can be that the partner’s attitude towards contraceptives would influences mother’s use of postpartum contraceptives.
The utilization of ANC service was not found to be a significant predicator of the use of contraception in the postpartum period. This study was supported by study conducted at North West Ethiopia Dabat district and in Thailand. However, this study was not supported by cross-sectional study conducted in Gonder town and Bahardar that revealed Women who had ANC visit during pregnancy were more likely utilize postpartum contraceptive than women who didn’t start ANC visit during pregnancy. The difference among these studies might be due to poor counseling during antenatal care visit on the importance of postpartum family planning use. The findings show that the use of a modern method of contraception during the postpartum period is significantly associated with providing FP education after delivery at health facilities level. This relationship is consistent with findings reported by other studies in India and Mexico. This might be mothers coming to PNC are more likely to obtain adequate counselling to the use PPFP at health facilities and create awareness on family planning related information from the health-care providers. The occurrence of problems with previous contraceptive utilizations shows that negatively associated with postpartum contraceptive use during the postpartum period. A study conducted in North Ethiopia and in Malawi supports this finding. This may be due to dissatisfaction of mothers in the service because of poor counseling of health provider in addition of fear of the occurrence of problems.
In this study, overall knowledge on PPFP is 100%. The finding of this study is similar with the study done in Northwest Ethiopia (98.31%). This shown that health workers are the primary source of contraceptive information at health institutions and home to home visits. Educational status (illiterate and literate) of Postpartum women was not found a statically significant predicator of the use of contraception in the postpartum period. This study was not supported study done in Eastern Ethiopia and in Northern Ethiopia. This might be due to difference in the socio-demographic characteristics, and the study included only urban populations. Previous Abortion of Postpartum women was found a statically significant predicator of the use of contraception in the postpartum period. This study was not supported study done in North West Ethiopia. This might be due to difference in culture, socio-demographic characteristics.
Conclusion
This study indicates that the prevalence of postpartum contraceptive utilization is low which is found to be 38.6%. Factors such as mother’s discussion with husbands on modern FP, number of pregnancy and duration of postpartum , Place where received FP counselling after delivery, experience any problem with modern family planning methods utilizations and experience of abortion were factors predict postpartum modern contraceptive utilization. The reasons for non-users of postpartum FP were wants to have more children and feeling not at risk due to breast feeding were the main factors. This requires effective response by Hawassa city health department to enhance the uptake of postpartum contraceptive through well-organized family planning education and follow up for the reproductive age women. Discussion about FP is crucial to improve mothers’ contraceptive utilization practice and changing the mothers’ knowledge to an action. So, health service providers should provide/promote contraceptive services and counseling during PNC, ANC, delivery, immunizations and home visits for postpartum women were recommended to enhance the prevalence of postpartum contraceptive utilization.
Limitations
Utilization status of postpartum modern family planning was determined at a point in time which may slightly lower the prevalence.
Ethical Approval
Ethical clearance and supportive letter were obtained from Hawassa pharma college school of post graduate Institutional Review Board (IRB). Written permission was obtained from the South Regional Health Bureau and Hawassa Town Health Department. Informed consent was directly obtained from study participants by explaining the objectives of the study. Confidentiality was assured for the information provided, Participation in the study was on voluntary bases and informed about the right not to participate or withdraw at any time without compromising their health services.
Consent for Publication
Not applicable.
Availability of Data and Materials
Data is not available for online access, however readers who wish to gain access to the data can write to the corresponding author Kebede Tefera.
Competing Interest
The authors declare that they have no competing interests.
Funding
The funding source of this research was Pharma College School of Post Graduate and College has no role in design, data collection, analysis, decision to publish as well as preparation of the manuscript.
Authors’ Contributions
KT and MA were involved in conception, designing the study, writing proposal, analysis, interpretation of data and manuscript writing. All authors agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Acknowledgment
We would like to thank Pharma College School of Post Graduate for funding this thesis work. My pleasure typically goes to study participants and data collectors for their valuable time, commitment and more of their support in all. We would like to show our appreciation for the South Regional Health Bureau and Hawassa Town Health Department in the process of data collection.
Author Information
Kebede Tefera: Lecturer, school of public health, college of medicine and health sciences, Hawassa university; Mulugeta Abuye: Expert on reproductive health, doctors with Africa CUAMM, Addis Ababa, Ethiopia.
References
- Conde-Agudelo A, Belizan JM (2000) Maternal morbidity and mortality associated with interpregnancy interval: Cross sectional study. Bio Med J 321: 1255-1259.
[Crossref] [Google Scholar] [PubMed]
- Smith R, Clifton D, Gribble, Ashford L (2009) Family planning saves lives. Population Refer Bureau 1: 25.
- Akinlo A, Bisiriyu A, Esimai O (2013) DHS working papers: Influence of use of maternal health care on postpartum contraception in Nigeria. Calverton, Maryland, USA: The DHS Program 92.
- Roy TK, Ram F, Nangia P, Saha U, Khan N (2003) Can women's childbearing and contraceptive intentions predict contraceptive demand? Findings from a longitudinal study in Central India. Int Family Plan Perspect 25-31.
[Crossref] [Google Scholar] [PubMed]
- Abera Y, Mengesha ZB, Tessema GA (2015) Postpartum contraceptive use in Gondar town, Northwest Ethiopia: A community based cross-sectional study. BMC Women's Health 15: 1-8.
- Jima GH, Garbaba WB (2020) Postpartum family planning utilization and associated factors among women who gave birth in the last 12 months prior to the study in lode Hetosa district, South East Ethiopia. J Women’s Heal Care 9.
- Adegbola O, Okunowo A (2009) Intended postpartum contraceptive use among pregnant and puerperal women at a university teaching hospital. Archiv Gynecol Obstetr 280: 987-992.
[Crossref] [Google Scholar] [PubMed]
- Haile A, Enqueselassie F (2006) Influence of women's autonomy on couple's contraception use in Jimma town, Ethiopia. Ethiopian J Health Develop 20.
- Mengesha ZB, Worku AG, Feleke SA (2015) Contraceptive adoption in the extended postpartum period is low in Northwest Ethiopia. BMC Pregnancy Childbirth 15: 1-6.
[Crossref] [Google Scholar] [PubMed]
- Shegaw M (2007) Assessment of the contraceptive needs and practice of women in the extended postpartum period, Ethiopia.
- Maternal morbidity and mortality associated with interpregnancy interval: Cross sectional study
- Zerai A, Tsui AO (2001) The relationship between prenatal care and subsequent modern contraceptive use in Bolivia, Egypt and Thailand. Afr J Reprod Health 5: 68-82.
[Crossref] [Google Scholar] [PubMed]
- Abraha TH, Tefera AS, Gelagay AA (2017) Postpartum modern contraceptive use in northern Ethiopia: Prevalence and associated factors. Epidemiol Health 39.
- Bwazi C, Maluwa A, Chimwaza A, Pindani M (2014) Utilization of postpartum family planning services between six and twelve months of delivery at Ntchisi District Hospital, Malawi Health.
- Anguzu R, Tweheyo R, Sekandi JN, Zalwango V, Muhumuza C, Tusiime S, et al. (2014) Knowledge and attitudes towards use of long acting reversible contraceptives among women of reproductive age in Lubaga division, Kampala district, Uganda. BMC Res Notes 7: 1-9.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences