Modern Contraceptive Utilization and Associated Factors among HIV Positive Women on Antiretroviral Therapy in Mizan-Tepi Teaching and Referral Hospital, South-West Ethiopia
Kindie Mitiku
DOI10.21767/2471-9749.100033
Kindie Mitiku* Sharew Mulugeta and Buraka Lemessa
Public Health, Mizan-Tepi University, Ethiopia
- *Corresponding Author:
- Kindie Mitiku
Lecturer, Mizan-Tepi University
Public Health, Ethiopia
Tel: +251917742402
E-mail: mitikukindie@gmail.com
Received Date: October 02, 2017; Accepted Date: October 10, 2017; Published Date: October 18, 2017
Citation: Mitiku K, Mulugeta S, Lemessa B (2017) Modern Contraceptive Utilization and Associated Factors among HIV Positive Women on Antiretroviral Therapy in Mizan-Tepi Teaching and Referral Hospital, South-West Ethiopia. J Contracept Stud Vol.2 No.2:10
Abstract
Background: Women living with human immunodeficiency virus encounter unintended pregnancy with related risk of mother to child transmission of HIV. Unintended pregnancy among these peoples is associated with inconsistence use of contraceptives. The aim of this study is to assess the prevalence of modern contraceptive utilization and associated factors in the Mizan-Tepi teaching and referral hospital. Methods: Hospital based cross-sectional study was conducted on 382 HIV positive reproductive age women who were on antiretroviral therapy. Data was gathered using pretested structured questionnaire in exit interview. Data was entered using Epidata version 3.1 and exported to SPSS version 21.0 for further analysis. Binary and multivariable analyses were done using SPSS. Results: Majority (98.2%) of women ever heard at least one type of modern contraceptives. However, only 64.1% of them were using modern contraceptives. Injectables (64.9%) and condoms (31.4%) were the most commonly used contraceptives whereas intrauterine devices and implants were used by only 2.4% and 9.8% of the participants respectively. Women whose age ≥ 35 years old (AOR=0.30; 95% CI: 0.09, 0.96), Muslims (AOR=0.34; 95% CI: 0.17, 0.67), widowed/ separated (AOR=0.21; 95% CI: 0.10, 0.45), monthly income ≥ 1500 birr (AOR=0.29; 95% CI 0.13, 0.69) and not having discussion with partner (AOR=0.18; 95% CI 0.07, 0.47) were less likely to use modern contraceptives. Whereas, women whose partner educational status secondary and above (AOR=2.78; 95% CI 1.22, 6.36) were more likely to use modern contraceptives. Conclusion: Modern contraceptive utilization is suboptimal. But, utilization of long acting contraceptives was found to be very low. Partner level of education and open discussion with partner were positively associated with contraceptive use. However, old age, being Muslim and being widowed/separated were negatively associated with current contraceptive use. Therefore, behavioral education and communication targeted on improving contraceptive use among HIV positive women need to address these factors.
Keywords
HIV positive; ART attendees; Contraceptive use and Family planning
Background
In 2013, an estimated 35.0 million people were living with human immune deficiency virus worldwide. Sub-Saharan Africa alone accounted for 71% of the global burden of HIV infection [1]. Women and children are disproportionally affected by HIV/ADIS. As estimated by UNAIDS, globally, 3.2 million children were living with HIV in the year 2013. Similarly, as of 2013, an estimated 16 million women aged 15 years and older were living with HIV and 80% of them live in sub-Saharan Africa. The adult prevalence of HIV in Ethiopia was estimated to be 1.1% in 2016 [2]. In Ethiopia, women are disproportionally affected by HIV/AIDS. The 2011 Ethiopian demographic and health survey showed that HIV prevalence in women was 1.9% which is higher than prevalence in men (1.0%) [3]. In sub-Saharan Africa, the main mode of HIV transmission is through heterosexual sex with a concomitant epidemic in children through vertical transmission [4]. Despite the risk of mother to child transmission of HIV, significant proportion of parents living with HIV continued to desire to have children [5-8]. Studies also revealed that HIV-positive women encountered unintended pregnancies with associated risk of mother to child transmission of HIV [9-11]. The experience of repeated untended pregnancy among HIV positive women particularly adolescents is partially due to inconsistence use of contraceptives [12].
The global prevention of mother to child transmission of HIV strategy advocates a four-pronged strategy of elimination of new HIV infections among children and keeping their mothers alive. The four pillars of the strategy are primary prevention of HIV infection, preventing unintended pregnancy among HIV-infected women, preventing HIV transmission from HIVinfected women to their infants, and care for HIV-infected mothers and their children [13]. One of the pillars of the strategy “preventing unintended pregnancy among HIV-infected women” could be addressed through effective contraceptive utilization. Effective contraceptive utilization could prevent unintended pregnancies among HIV/AIDS patient. In fact, the effectiveness of contraceptive use in preventing HIV positive births has already been established [14].
Despite its potential benefit, significant proportions of women in many sub-Saharan African countries including Ethiopia don’t use modern contraceptives. For instance, in Kumsia Ghana only 42.6% of women living with HIV/AIDS were reported to use modern contraceptives in 2014 [15]. Further analysis of the Malawi demographic health survey in 2015 also revealed that only 51.2% of women living with HIV/AIDS used modern contraceptives [16].
Studies in South-west Uganda [17] and three other districts of Uganda namely Wanyenze et al. [18] revealed that 28.8% and 68% of women living with HIV/AIDS used modern contraceptives respectively.
In Ethiopia, studies suggested that modern contraceptive utilization among women living with HIV/AIDS various from region to region. For instance, it was reported as high as 80% in Bahir Dar in 2015 [19]. While coverage was as low as 47% in Debremarkos [20], 44.3% in Tigray [21], 61.6% in Nekemte hospital [22] and 56.7% in Gimbe town [23]. However, the prevalence of modern contraceptive utilization among women living with HIV/AIDS is better than general population. The most recent EDHS estimated that the national and regional (South nation nationalities and peoples region) prevalence of modern contraceptives among the general population was 35% and 39.6%, respectively [24].
Various factors have been reported to be associated with utilization of modern contraceptives among women living with HIV/AIDS. Studies revealed that there is significant difference in the utilization of modern contraceptives between educated and uneducated women. Educated women are more likely to use modern contraceptives than uneducated women [25,26]. Particularly, women who completed primary and secondary education are more likely to use modern contraceptives. There is also urban-rural difference in contraceptive utilization. Those women who reside in urban areas use contraceptives more likely than their counterpart. In fact, women residing in remote and rural areas are less likely to use modern contraceptives due to distance barriers. Some studies revealed that there is significant variation in utilization of modern contraceptives among poor and rich women living with HIV/AIDS where women from the rich wealth quintile and having higher income are more likely to use modern contraceptives. Socio-demographic profile of women such as marital status [27], number of children and age of women also influence women utilization of modern contraceptives. There is positive relation between marital status and modern contraceptive utilization in which married women are more likely to use modern contraceptives. The numbers of children the couples would have also influence women access to modern contraceptives. Women who have more numbers of children are more likely to use modern contraceptives. Some studies argued that as women’s age increase the likelihood to use modern contraceptive decrease [28].
Information on the available options of modern contraceptive and where they found is crucial for women to access and use contraceptives. Studies suggested that women who discussed about family planning with providers are more likely to use modern contraceptives [29]. Not only discussing with providers but also discussing with spouse increase women probability of using modern contraceptives .In fact, women who decide jointly are more likely to use modern contraceptive than who decide alone.
Despite several studies in sub-Saharan Africa and Ethiopia, there are scarce studies in the most remote region of Ethiopia like that of this study area. Up to the level of investigators knowledge, this study is the first attempt in remote South-west Ethiopia and aimed to assess the magnitude of modern contraceptive utilization and associated factors among women living with HIV/ AIDS who were on HAART in Mizan-Tepi university teaching and referral hospital.
Methods
Study area and period
This study was conducted in Mizan-Tepi university teaching and referral hospital starting from July to august 2016 G.C. Mizan-Tepi university teaching and referral hospital is found in Bench Maji Zone, South-west region of Ethiopia which is 561 km away from Addis Ababa. This hospital was established in 1987 GC and currently serving an estimated total population of 760,314 [30].
Study design, source and study populations
Hospital based cross-sectional study was conducted. The source populations were HIV positive reproductive age women enrolled in HIV/AIDS care at ART clinic in Mizan-Tepi university teaching and referral hospital. On the other hand our study populations were HIV positive reproductive age women enrolled in HIV/AIDS care at ART clinic in Mizan-Tepi University teaching and referral hospital that was included in the study.
Sample size determination and sampling procedure
The minimum sample size was computed by using single population formula based on the following assumptions: the prevalence of modern contraceptive utilization (61.6%) taken from previous study; Z-value at 95% confidence level (CI) 1.96; and 5% margin of error. By adding 10% non-response rate, the final sample size was 400. All women that fulfil the inclusion criteria were interviewed consecutively.
Inclusion and exclusion criteria
Married or cohabiting reproductive aged women (15-49 years old) and women who were sexually active one year prior to our survey was included. However, those women who were severely ill and admitted for inpatient management were excluded. Furthermore, in fecund women were excluded.
Data collection tools and procedure
A pre-tested structured questionnaire was used. The questionnaire was derived from related questions in the Demographic Health Survey and other related literatures [31]. The data collection tool (questionnaire) was prepared first in English and then translated to Amharic which is spoken by the local peoples and then retranslated back to English language. The pretest was conducted on 19 women in the same city but different health institution (i.e., at Mizan health center). After pretest; grammatical errors, logical flow of the questioners was corrected. Three public health gradated students collected the data. The primary investigators supervise the data collection process. Data collectors were trained on the tool and the procedure by principal investigator. Data were gathered through an exit interview outside the ART clinic.
Operational Definitions
Current use of contraceptive method: Referred to respondents who responded positively for use of at least one type of contraceptive methods at time of the survey to delay or avoid pregnancy.
Modern contraceptives: Contraceptive method queries included male and female condoms (restricted to those reporting ‘‘Always’’ use), injections (depo medroxy progesterone acetate (DMPA) or norethisterone enantate), oral contraceptive pills, diaphragm, intrauterine devices (IUD), female tubal ligation, hysterectomy, and male partner sterilization.
Sexually active: Women who had sexual practice during the last one year before interview was labeled as sexually active.
Cohabiting with partner: Referred to women responded as they are living in union but legal marriage has not established.
In Fecund: Women who never used contraception, and not had a birth in past five years, reported as they ‘‘can’t get pregnant’’ or have had a hysterectomy were considered in fecund for this study.
Data processing and analysis: The data were checked, coded and entered in to Epidata version 3.1 and exported to SPSS version 21.0 for analysis. Using SPSS, Proportions and medians were computed as univariate analysis. Furthermore, bivariate analysis and Multivariable analysis were done. Each variable was first analyzed by using bivariate logistic regression (bivariate analysis) and covariates having p-value less than 0.2 was further entered in to multivariable logistic regression model for final analysis. Multivariable analysis was done using ‘enter’ method. In the multivariable analysis, P-value less than 0.05 was used as a statistical significant and odds ratio with 95% CI was used to assess the presence and strength of association between covariates and dependent variable. The multivariable logistic regression model explained 38.7% (Nagekeke R square) of the variance in modern contraceptive utilization. Hosmer lomeshow goodness of test was done to assess fitness of the model. Hosmer lomeshow test greater or equal to 0.05 was considered to ensure goodness of fit of the model.
Ethical approval: Ethical clearance was obtained from research community development and support office of Mizan-Tepi University. Official permission letter was collected from the office of Mizan- Tepi teaching and referral hospital. Verbal consent was obtained from each study participants. All the study participants were informed about the objective and importance of the study and were also informed about their right not to participate or withdraw from the study at any time. Confidentiality was assured by conducting interviews in a private room out of the ART clinic. Data were password protected and stored on computers that was accessed only by the principal investigators.
Results
Socio-demographic characteristics
A total of 382 women were participated in this study yielding a response rate of 95.5%. About 18 women refused to participate in this study. The reasons for not participating were not directly linked to the study. The median age of study participants were 30.0 years old with IQR of (15, 45 years old). Majority of the participants 314 (82.2%) were urban residents and orthodox religion 223 (58.4%) followers. Nearly seventy percent (68.3%) of women were married and 222(58.2%) attended formal education. Of the total participants, 240(63.4%) had more than one child. The median monthly income of participants was 1000.00birr IQR (100birr, 9000birr) (Table 1).
| Characteristics | Categories | Frequency (n) | Percent |
|---|---|---|---|
| Age at interview in years | 15-24 25-34 |
45 190 |
11.8 49.7 |
| Median=30.0 years oldIQR(15, 45) | ≥35 | 144 | 37.7 |
| Residence | Urban | 314 | 82.2 |
| Rural | 68 | 17.8 | |
| Religion | Orthodox | 223 | 58.4 |
| Muslim | 88 | 23 | |
| Protestant | 71 | 18.6 | |
| Women educational status | No formal education | 160 | 41.9 |
| Primary education(1-8) | 179 | 46.9 | |
| Secondary and above(≥ 9) | 43 | 11.3 | |
| Current marital status | Married | 261 | 68.3 |
| Never married /single | 21 | 5.5 | |
| Widowed/separated/divorced | 100 | 26.2 | |
| Partner level of education | No formal education | 135 | 35.3 |
| Primary level education(1-8) | 117 | 30.6 | |
| Secondary and above(≥ 9) | 72 | 18.8 | |
| Parity(number of children) | <1 | 140 | 36.6 |
| 01-Apr | 212 | 55.5 | |
| ≥5 | 30 | 7.9 | |
| Number of currently alive children | <1 | 152 | 39.8 |
| 01-Apr | 209 | 54.7 | |
| ≥5 | 21 | 5.5 | |
| Monthly income | ≤500 ETB | 103 | 27 |
| 500-1500 ETB | 189 | 49.5 | |
| Median 1000.00ETB IQR(100, 9000ETB) | ≥ 1500ETB | 83 | 21.7 |
Note: ETB: Ethiopian Birr; IQR: Inter Quartile Range.
Table 1 Socio-demographic characteristics of HIV positive reproductive age women who were on HAART Mizan-Tepi teaching and referral hospital, 2017.
HIV related characteristics of study participants
Nearly three quarter 255 (66.8%) of women’s index child HIV status was positive. Majority of women 320 (83.8%) exposed their HIV status to their husband or partner. Almost all women 366 (95.8%) heard about mother to child transmission of HIV/ AIDS. About 366 (95.8%), 202 (52.9%) and 140 (36.6%) of women mentioned that HIV could transmit from mother to child during pregnancy, child birth and breast feeding respectively Table 2.
| Characteristics | Categorization | Frequency | Percent |
|---|---|---|---|
| HIV status of young child | HIV positive | 74 | 19.4 |
| HIV negative | 255 | 66.8 | |
| Not tested | 14 | 3.7 | |
| Exposed her HIV status to partner | Yes | 320 | 83.8 |
| No | 62 | 16.2 | |
| Knew HIV status of partner/husband | Yes | 288 | 75.4 |
| No | 94 | 24.6 | |
| Aware about MTCT of HIV | Yes | 366 | 95.8 |
| No | 16 | 4.2 | |
| When does HIV transmit from mother to baby? | During pregnancy | 319 | 83.5 |
| During child birth | 202 | 52.9 | |
| During breast feeding | 140 | 36.6 | |
| Aware about the presences of medicine that prevent MTCT of HIV | Yes | 331 | 86.6 |
| No | 51 | 13.4 |
Note: HIV-Human Immune Deficiency Virus, MTCT; Mother to Child Transmission.
Table 2 HIV related characteristics of women who were on HAART in Mizan-Tepi teaching and referral hospital, 2017.
Information on modern contraceptives and contraceptive utilization
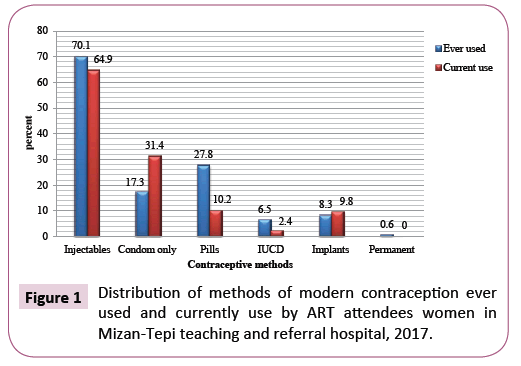
Among 382 study participants, nearly all of them 375 (98.2) have mentioned hearing about at least one type of modern contraceptive from various sources. The highest proportion of women 295 (77.2%) heard from health professionals. Concerning information about specific methods of modern contraceptive; injectables (94.5%), pills (94.1%) and condom (84.0%) were the most commonly known types of modern contraceptives. Majority (86.1%) of them ever got information about modern contraceptives from ART clinics. Majority study participants 324 (84.8) ever used at least one type of modern contraceptives. But, only 73 (19.1%) of them ever got modern contraceptives from ART clinic (Table 3). Nearly three quarter 245 (64.1%) of women were using modern contraceptives at the time of data collection. Injectables (70.1%), condoms (31.4%) and pills (27.8) were the major modern contraceptives used by study participants (Figure 1).
| Characteristics | Categorization | Frequency | Percent |
|---|---|---|---|
| Ever heard about modern contraceptives | Yes | 375 | 98.2 |
| No | 7 | 1.8 | |
| Source of information | Health professional | 295 | 77.2 |
| Radio/television | 56 | 14.7 | |
| Friends | 9 | 2.4 | |
| Relatives | 13 | 3.4 | |
| Others* | 2 | 0.5 | |
| Methods respondent heard about | Condom | 321 | 84 |
| Pills | 354 | 94.1 | |
| Injectables | 361 | 94.5 | |
| IUCD | 228 | 59.7 | |
| Norplant | 111 | 29.1 | |
| Permanent | 19 | 5 | |
| Ever got information from ART clinic | Yes | 329 | 86.1 |
| No | 53 | 13.9 | |
| Methods respondent ever heard from ART clinic | Condom | 268 | 70.2 |
| Pills | 320 | 83.8 | |
| Injectables | 316 | 82.7 | |
| IUCD | 203 | 53.1 | |
| Norplant | 133 | 34.8 | |
| Permanent | 33 | 8.6 | |
| Ever used contraceptive method | Yes | 324 | 84.8 |
| No | 58 | 15.2 | |
| Ever got contraceptive method from ART clinic | Yes | 73 | 19.1 |
| No | 309 | 80.9 | |
| Current use | Yes | 245 | 64.1 |
| No | 137 | 35.9 | |
| Reasons for not using contraceptive Currently | Want to have child in the future | 52 | 38 |
| In frequent sexual intercourse | 78 | 56.9 | |
| Lack of awareness | 1 | 0.7 | |
| Against my religion | 1 | 0.7 | |
| My husband don’t allow | 3 | 2.2 | |
| Others** | 2 | 1.5 | |
| Discussed about contraceptive with partner | Yes | 334 | 87.4 |
| No | 48 | 12.6 | |
| Decision making power on contraception | Women only | 40 | 10.5 |
| Husband only | 19 | 5 | |
| Jointly | 323 | 84.6 | |
| Family planning services should be given at ART clinic | Agree | 363 | 95 |
| Disagree | 19 | 5 |
Note: HAART–Highly Active Anti-Retroviral Therapy, IUCD: Intrauterine Devices.
*Leaflets/magazines, **Fear of side effect, Causes infertility.
Table 3 Information on modern contraceptives and contraceptive use among female HAARTattendees in Mizan-Tepi teaching and referral hospital, 2017.
About 35.9% of women were not using contraceptive at the time of data collection. Want to have child in the future (38.0%) and infrequent sexual intercourse (56.9%) were the main reasons mentioned by study participants.
Bivariate and multivariable analysis
Without controlling potential confounders; age of women, religion, current marital status, number of total and alive children, monthly income, discussion about modern contraceptive with partner or husband, knowing the HIV status of partner and HIV status exposure were significantly associated with current modern contraceptive use (Table 4). After controlling potential confounders; age of women, religion, current marital status, partner level of education, monthly income and discussion with partner about modern contraceptive remain significantly associated with modern contraceptive use. At Multivariable level; The odds of using modern contraceptives for women whose age ≥ 35 years old was 70% less likely as compared to women whose age was between 15 and 24 years old. Muslims were 66% less likely to use modern contraceptive compared to orthodox religion followers. Similarly, widowed or separated women were 79% less likely to use modern contraceptive compared to married women. Women who didn’t discuss about modern contraceptive with partner were 82% less likely to use modern contraceptive. Furthermore, the odds of modern contraceptive utilization among women whose monthly income ≥ 1500 birr were71% less likely as compared with women whose monthly income ≤ 500 birr.
| Characteristics | Categories | Contraceptive use | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age at interview in years* Median = 30.0 IQR(15, 45) |
15-24 25-34 ≥ 35 |
33 (73.3%) 136 (71.6%) 74 (51.4%) |
12 (26.7%) 54 (28.4%) 70 (48.6%) |
1 0.92 (0.44-1.90) 0.38 (0.18-0.80)* |
1 0.80 (0.27-2.34) 0.30 (0.09-0.96)** |
| Residence | Urban Rural |
207 (65.9%) 38 (55.9%) |
107 (34.1%) 30 (44.1%) |
1 0.66 (0.38-1.12) |
1 0.70 (0.32-1.51) |
| Religion | Orthodox Muslim Protestant |
159 (71.3%) 45 (51.1%) 41 (57.7%) |
64 (28.7%) 43 (48.9%) 30 (42.3%) |
1 0.421 (0.25-0.70)* 0.550 (0.32-0.96)* |
1 0.34 (0.17-0.67)** 0.49 (0.21-1.13) |
| Women educational status | No formal education Primary(1-8) Secondaryand above(≥ 9) |
98 (61.3%) 120 (67.0%) 27 (62.8%) |
62 (38.8%) 59 (33.0%) 16 (37.2%) |
1 1.287 (0.82-2.01) 1.068 (0.53-2.14) |
|
| Current marital status | Married Single Widowed/separated |
195 (74.7%) 15 (71.4%) 35 (35.0%) |
66 (25.3%) 6 (28.6%) 65 (65.0%) |
1 0.85 (0.32-2.27) 0.18 (0.11-0.30)* |
1 0.40 (0.05-3.17) 0.21 (0.10-0.45)** |
| Partner education status | No formal education Primary education Secondary& above (≥ 9) |
87 (64.4%) 72 (61.5%) 55 (76.4%) |
48 (35.6%) 45 (38.5%) 17 (23.6%) |
1 0.88 (0.53-1.47) 1.79 (0.93-3.41) |
1 1.190 (0.61-2.34) 2.783 (1.22-6.36)* |
| Parity | <1 1-4 ≥ 5 |
88 (62.9%) 144 (67.9%) 13 (43.3%) |
52 (37.1%) 68 (32.1%) 17 (56.7%) |
1 1.25 (0.79-1.96) 0.45 (0.20-1.01) |
1 2.13 (0.43-10.45) 1.57 (0.17-14.86) |
| Currently alive children | <1 1-4 ≥ 5 |
98 (64.5%) 141 (67.5%) 6 (28.6%) |
54 (35.5%) 68 (32.5%) 15 (71.4%) |
1 1.14 (0.74-1.78) 0.22 (0.08-0.60)* |
1 0.61 (0.13-2.88) 0.73 (0.06-8.72) |
| Monthly income | ≤500 ETB 500-1500 ETB ≥ 1500ETB |
66 (64.1%) 134 (70.9%) 41 (49.4%) |
37 (35.9%) 55 (29.1%) 42 (50.6%) |
1 1.37 (0.82-2.28) 0.55 (0.30-0.99)* |
1 1.55 (0.74-3.26) 0.29 (0.13-0.69)** |
| Ever got information from ART clinic | Yes No |
216 (65.7%) 29 (54.7%) |
113 (34.3%) 24 (45.3%) |
1 0.63 (0.35-0.14)* |
1 1.02 (0.45-2.32) |
| Discussed about contraceptive with partner | Yes No |
228 (68.3%) 17 (35.4%) |
106 (31.7%) 31 (64.6%) |
1 0.26 (0.14-0.48)* |
1 0.18 (0.07-0.47)** |
| Ultimate decision power on contraception | Women only Husband only Jointly |
25 (62.5%) 13 (68.4%) 207 (64.1%) |
15 (37.5%) 6 (31.6%) 116 (35.9%) |
1 1.30 (0.41-4.14) 1.07 (0.54-2.11) |
|
| Exposed her HIV status to partner | Yes No |
221 (69.1%) 24 (38.7%) |
99 (30.9%) 38 (61.3%) |
1 0.28 (0.16-0.49)* |
1 0.83 (0.26-2.71) |
| Knew HIV status of partner | Yes No |
205 (71.2%) 40 (42.6%) |
83 (28.8%) 54 (57.4%) |
1 0.30 (0.19-0.49)* |
1 0.42 (0.15-1.16) |
| Aware about MTCT of HIV | Yes No |
237 (64.8%) 8 (50.0%) |
129 (35.2%) 8 (50.0%) |
1 0.54 (0.20-1.48) |
|
| Aware the presences of medicine that prevent MTCT of HIV | Yes No |
214 (64.7%) 31 (60.8%) |
117 (35.3%) 20 (39.2%) |
1 0.85 (0.46-1.55) |
|
Note: IQR: Inter Quartile Range, COR: Crude Odd Ratio, AOR: Adjusted Odd Ratio, CI: Confidence Interval.
*Significant at bivariate analysis, **Significant at multivariable analysis, 1: Reference category.
Table 4 Factors associated with current modern contraceptive use among HIV positive women on antiretroviral therapy in Mizan-Tepi teaching and referral hospital, 2017.
Discussion
This study tried to assess modern contraceptive utilization and associated factors among HIV positive women who were on HAART at the time of the study in Mizan-Tepi teaching and referral hospital. This study is the first attempt in this remote teaching and referral hospital.
Congruent with other studies in developing countries nearly all of the study participants ever heard at least one type of modern contraceptives. Over all, more than half of married or sexually active women were using at least one type modern contraceptives. This finding is higher than the regional (39.8%) and national (35.0%). Prevalence of modern contraceptive utilization. The higher prevalence of modern contraceptive utilization in this study area as compared to the national and regional estimate might be due to study population difference. The regional and national estimate of modern contraceptive was from the general population where as our estimate was from HIV positive women who were on HAART. Previous studies revealed that modern contraceptive utilization is relatively higher among HIV positive women as compared to the general population [32]. Our finding is also higher than other studies conducted in various parts of Ethiopia such as Debremarkos (47.9%) and Northern Tigray (44.3%). The possible explanation for low utilization of modern contraceptives in these areas might be difference in study period and eligibility criteria. In our study, all participates had started HAART. Whereas, study participants in other studies (Debremarkos and Northern Tigray) were either who started HAART or pre-HAART HIV patients. Studies have found that modern contraceptive utilization is relatively higher among women who started HAART than pre-HAART women [33]. Similarly, the findings of this study is higher than studies conducted in other developing countries such as in Kumesia Ghana (42.6%), Democratic republic of Congo (35.5%) [34] and Malawi (51.2%). This might be due to geographical and study period difference. In contrary, our finding was relatively lower than study findings from Uganda (85%) [35] and Bahir Dar (80%). This variation might be due to study population and inclusion criterion difference. For instance, majority of the study populations in Bahir Dar (92.3%) were urban whereas in this study 82.2% of the participants were urban which is relatively lower than study conducted in Bahir Dar. It has been documented that urban populations are more likely to use modern contraceptive than rural counterparts.
Furthermore, a study conducted in Uganda included self-reported use of family planning in the previous 3 months to measure contraceptive use which is longer period as compared to this study. In this study, we measured current level of contraceptive. This in turn might decrease prevalence of contraceptive use in our study.
Even though modern contraceptives were available at free cost in ART clinic of this study setup, still significant proportion of women were not using modern contraceptives. This was because of desire to have children in the future and infrequent sexual practice which is broadly in line with several studies. Studies have shown that women who have desire of children in future are less likely to use modern contraceptives. In fact, women living with HIV have strong desire of children due to the availability of drugs that prevent mother to child transmission of HIV [36].
The most commonly used methods of modern contraceptive were injectables and condoms. Similarly, other studies in Ethiopia and sub-Saharan Africa revealed that women living with HIV preferred condom and injectables than long acting contraceptives such as implants and IUCD. In this study, small proportion of study participants used long acting contraceptive methods. This could be due to provider bias, poor method mix or contraceptive related myths. A study in Bahir Dar concluded that there is high unmet need of long acting contraceptives among women living with HIV/AIDS. This study argues that myths related to long acting contraceptives contribute for low utilization of long acting contraceptives. Despite majority of study participants wanted contraceptives to be given at ART clinics, only small proportion of women got contraceptives from ART clinic. This might be due to unavailability of method mix or trained family planning provider at ART clinic.
This analysis identifies individual and household level factors; age of women, marital status, religion affiliation, partner level of education, open discussion with partner and monthly income significantly associated with experience of modern contraceptive use among women living with HIV/AIDS who were on HAART. Women who were divorced, separated or widowed were less likely to use modern contraceptive than married women. A similar finding was reported in Tigray. This could be partially explained by infrequent sexual practice among these segments of women. This could be more likely true because further analysis of our data depicts that 38.9% widowed, separated or divorced women mentioned that their reason for not using modern contraceptive was infrequent sex.
Despite high fertile desire among young women, we found that old women were less likely to use modern contraceptives as compared to young women. The observed association of decreased use of contraception with increased age is in line with previous findings of lower modern contraceptive use among older women on ART in Zambia [37] and HIV-infected women in Uganda. In this study, Muslim women were 80% less likely to use modern contraceptives than Christians. This finding is in agreement with study conducted in Kersa, Ethiopia [38]. This might be due to the wide belief in the Muslim community that considers family planning prohibited in the holly book. Another finding of this study is, those women whose partner level of education above secondary level were more likely to use modern contraceptive than illiterate partners. Education may increase partners’ level of knowledge on HIV status and ways of transmission. In other study, it is documented that partner knowledge on HIV status contributes contraceptive utilization. Furthermore, open discussion with partner was found to be significantly associated with contraceptive utilization. The positive association of open discussion with partner and contraceptive utilization was documented in the broader literatures. Open discussion with partner may enable women to make informed decision on fertility and contraceptive options. In fact, Discussion of HIV status among couples may be easier when they have disclosed their HIV status. In this study, women who had higher monthly income (≥ 1500 ETB) were less likely to use modern contraceptive than those who had <500 ETB. This finding is contrary to study finding in South-western Uganda. Women who had higher monthly income have high decision to have children [39] and people living with HIV/AIDS who had better income may feel that they could have the opportunity for better care of their child.
Limitation of the Study
This study was cross-sectional in nature. So it is difficult to determine the direction of causality between explanatory variables and current use of modern contraceptives. We tried to decrease the risk of social disability bias by interviewing women outside the ART clinic. However, some women might overreport their contraceptive use because of pressure from health workers and community members to practice protected sex. Though there are wide ranges of factors which affect utilization of contraceptive methods among HIV positive women, only individual and household level factors were addressed in this study. Hence, considering factors from the service providers’ side and structural barriers would have been important.
Furthermore, male were not interviewed in this study. Thus, the views of husband on contraceptive use were not captured. Therefore, future research that focused on contraceptive use among HIV/AIDS patients in this area need to address these limitations.
Conclusion
Awareness on at least one type of contraceptive was universal. However, current modern contraceptive utilization was found to be suboptimal. Particularly, utilization of long acting contraceptives was very low. The chance of current modern contraceptive utilization decreases with increasing age and monthly income. But, it increases with level of partner education. Religious affiliation (being Muslim) and not discussing with partner about contraceptives were associated with reduction in the chances of being current user of modern contraceptives. Moreover, being separated or widowed were negatively associated with current modern contraceptive use. Despite majority of women wanted contraceptives to be given at ART clinic, small proportion of women ever got contraceptives from ART clinic, suggesting poor integration of family planning with ART services.
Recommendations
i. Additional efforts are needed to promote utilization of long acting contraceptive methods.
ii. Hospital managers and clinical officers need to consider integration of family planning with ART services not only in terms of awareness creation but also actual contraceptive services provision.
iii. Behavioral education and communication designed to promote modern contraceptive use in this study area need to be inclusive and focused on special groups of peoples like Muslims and women who are widowed or separated.
iv. Further exploration on the structural and provider side determinants of contraceptive use among HIV positive women is recommended.
Acknowledgment
We would like to acknowledge Mizan-Tepi University for its financial support in undertaking this research. Our special gratitude also goes to Mizan-Tepi teaching and referral hospital health management information system officers for providing the necessary back ground information. We would like to extend our appreciation to all data collectors and study participants for giving us their time during the entire study period.
Competing Interests
The authors declare that they have no competing interests.
References
- Joint United Nations Programme on HIV/AIDS (UNAIDS) 2013. UNIIDS Report on the Global Epidemic 1: 145.
- Ethiopian Public Health Institute Federal & Ministry of Health(2014). HIV Related Estimates and Projections for Ethiopia 11: 6.
- Addis Ababa and Ethiop Calverton(2012) Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey, Maryland, USA. 89: 450.
- Kharsany ABM, Karim QA (2016) HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities. Open AIDS J34: 48.
- Wanyenze RK, Wagner GJ, Tumwesigye NM, Nannyonga M and Wabwire-mangen F,et al. (2013) Fertility and Contraceptive Decision-Making and Support for HIV infected IndividualsÃÆâÃâââ¬Ãâï: Client and Provider Experiences and Perceptions at Two HIV Clinics in Uganda. BMC Public Health 1: 11.
- Berhan Y, Berhan A (2013)Meta-Analyses of Fertility Desires of People Living with HIV. BMC Public Health 1: 8.
- Wagner GJ, Wanyenze R (2013). Fertility Desires and Intentions and the Relationship to Consistent Condom Use and Provider Communication Regarding Childbearing Among HIV Clients in Uganda. ISRN Infect Dis 1: 13.
- Regassa T, Fantahun M (2012). Fertility Desire and Reproductive Health Care Needs of Men and Women Living with HIV/AIDS in Nekemte, East Wollega, Ethiopia. Sci Technol Arts Res J31: 8.
- Homsy J, Bunnell R, Moore D, King R, Malamba S, et al. (2009) Reproductive Intentions and Outcomes Among Women on Antiretroviral Therapy in Rural UgandaÃÆâÃâââ¬Ãâï: A Prospective Cohort Study. PLoS One1: 10.
- King R, Khana K, Nakayiwa S, Katuntu D, Homsy J, et al. (2011) Pregnancy Comes Accidentally - Like it did with meÃÆâÃâââ¬Ãâï: Reproductive Decisions Among Women on ART and their Partners in Rural Uganda. BMC Public Health1: 11.
- Schwartz SR, Rees H, Mehta S, Daniel W, Venter F,et al. (2012) High Incidence of Unplanned Pregnancy After Antiretroviral Therapy InitiationÃÆâÃâââ¬Ãâï: Findings from a Prospective Cohort Study in South Africa. PLoS One1: 8.
- Obare F, Kwaak A Van Der, Birungi H (2012) Factors Associated with Unintended Pregnancy , Poor Birth Outcomes and Post-Partum Contraceptive use Among HIV-Positive Female Adolescents in Kenya. BMC Womens Health 1: 8.
- World Health Organization (2002). Strategic Approaches HIV Infection in Infants. Rep a WHO Meet Morges, Switz5: 20.
- Reynolds HW, Janowitz B, Wilcher R, Cates W (2008) Contraception to Prevent HIV-Positive Births: Current Contribution and Potential Cost Savings in PEPFAR Countries. Sex Transm Infect 49: 53.
- Laryea DO, Amoako YA, Spangenberg K, Frimpong E, Kyei-ansong J, et al. (2014) Contraceptive Use and Unmet Need for Family Planning Among HIV Positive Women on Antiretroviral Therapy in Kumasi , Ghana. BMC Womens Health 1: 8.
- Habte D, Namasasu J (2015) Family Planning Use Among Women Living with HIVÃÆâÃâââ¬Ãâï: knowing HIV Positive Status Helps - Results from a National Survey. Reprod Health1: 11.
- Muyindike W, Fatch R, Steinfield R, Matthews LT, Musinguzi N, et al. (2012) Contraceptive Use and Associated Factors Among Women Enrolling into HIV Care in Southwestern Uganda. Infect Dis Obstet Gynecol 1: 10.
- Wanyenze RK, Tumwesigye NM, Kindyomunda R, Beyeza-kashesya J, Atuyambe L, et al. (2011) Uptake of family planning Methods and Unplanned Pregnancies Among HIV-Infected IndividualsÃÆâÃâââ¬Ãâï: a Cross-Sectional Survey Among Clients at HIV Clinics in Uganda. J Int AIDS Soc1: 11.
- Kebede HG, Nahusenay H, Birhane Y (2015) Assessment of Contraceptive Use and Associated Factors among HIV Positive Women in Bahir-Dar Town , Northwest Ethiopia. Open Access Libr J 1: 19.
- Egzeabher SG, Bishaw MA, Tegegne TK, Boneya D (2015) Modern Family Planning Utilization and Associated Factors Among HIV Positive Reproductive Age Women in Debre Markos Referral Hospital Northwest Ethiopia, Open J Epidemiol 32: 40.
- Melaku YA, Zeleke EG (2014) Contraceptive Utilization and Associated Factors Among HIV Positive Women on Chronic Follow Up Care in Tigray Region , Northern EthiopiaÃÆâÃâââ¬Ãâï: A Cross Sectional Study. PLoS One 1: 10.
- Feyissa TR, Melka AS (2014) Demand for Modern Family Planning Among Married Women Living with HIV in Western Ethiopia. PLoS One1: 7.
- Polisi A, Gebrehanna E, Tesfaye G, Asefa F (2014) Modern Contraceptive Utilization Among Female ART Attendees in Health Facilities of Gimbie Town, Reprod Health1: 6.
- Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report 16: 24.
- Agadjanian V, Hayford SR, Luz L, Yao J (2015) Bridging User and Provider PerspectivesÃÆâÃâââ¬Ãâï: Family Planning Access and Utilization in Rural Mozambique. Int J Gynecol Obstet 47: 51.
- Nattabi B, Li J, Thompson SC, Orach CG, Earnest J, et al. (2011) Family Planning Among People Living with HIV in Post-Conflict Northern UgandaÃÆâÃâââ¬Ãâï: A Mixed Methods study. Confl Health 1: 12.
- Berhane Y, Berhe H, Abera GB, Berhe H (2013)Utilization of Modern Contraceptives Among HIV Positive Reproductive Age Women in Tigray , EthiopiaÃÆâÃâââ¬Ãâï: A Cross Sectional Study. ISRN AIDS 1: 8.
- Chibwesha CJ, Li MS, Matoba CK, Mbewe RK, Chi BH, et al. (2011) Modern Contraceptive and Dual Method Use Among HIV-Infected Women in Lusaka , Zambia. Infect Dis Obstet Gynecol 1: 8.
- Berhane Y, Kidanemariam A, Buruh G, Gegziabher G, Berhe H, et al. (2013) Utilization and Associated Factors of Modern Contraceptives Among HIV Positive Reproductive Age Women Attending Art Clinics in zonal Hospitals of Tigray region, North Ethiopia. Adv Res Pharm Biol 472: 80.
- Chakrapani V, Kershaw T, Shunmugam M, Newman PA, Cornman DH,et al. (2011) Prevalence of and Barriers to Dual-Contraceptive Methods Use among Married Men and Women Living with HIV in India. Infect Dis Obstet Gynecol 1: 9.
- Benchi-maji Zone Health office. Annual Performance Report. Unpublished 2017. 1: 34.
- Gelagay AA, Koye DN, Yeshita HY (2015) Demand for Long Acting Contraceptive Methods Among Married HIV Positive Women Attending Care at Public Health Facilities at Bahir Dar City, Northwest Ethiopia. Reprod Health 1: 9.
- Bankole A, Keogh S, Akinyemi O, Dzekedzeke K, Awolude O,et al. (2014) Differences in Unintended Pregnancy, Contraceptive Use and Abortion by HIV Status Among Women in Nigeria and Zambia. Int Perspect Sex Reprod Health 28: 38.
- Feyssa MD (2015) Unmet Need for Family Planning Among Women in HIV/AIDS Care at Antiretroviral Treatment Clinic in South Ethiopia: A Challenge to Prevention of Mother to Child Transmission. J AIDS Clin Res 1: 6.
- Yotebieng M, Norris A, Chalachala JL, Matumona Y, Ramadhani HO,et al. (2015) Fertility Desires, Unmet Need for Family Planning, and Unwanted Pregnancies Among HIV-infected Women in Care in Kinshasa,Pan Afr Med J 1: 8.
- Andia I, Kaida A, Maier M, Guzman D, Emenyonu N,et al. (2009) Highly Active Antiretroviral Therapy and Increased Use of Contraceptives Among HIV-Positive Women During Expanding Access to Antiretroviral Therapy in Mbarara, Uganda. Am J Public Health 340: 7.
- Getachew M, Alemseged F, Abera M, Deribew A (2010) Factors Affecting Fertility Decisions of Married Men and Women Living with HIV in South Wollo Zone, Northeast Ethiopia. Ethiop J Heal Dev 204: 20.
- Musa A, Assefa N, Weldegebreal F, Mitiku H, Teklemariam Z, et al. (2016) Factor Associated with Experience of Modern Contraceptive Use Before Pregnancy Among Women Who Gave Birth in Kersa HDSS , Ethiopia. BMC Public Health 1: 6.
- Rutenberg BN, Biddlecom AE, Kaona FAD (2000) Reproductive Decision-Making in the Context of HIV And AIDSÃÆâÃâââ¬Ãâï: A Qualitative Study in Ndola , Zambia. Int Fam Plan Perspect 124: 30.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences