Factors Influencing Utilization of Modern Contraceptive Methods among Rural Youths in Northern Uganda
Eustes Kigongo1*, Maxson Kenneth Anyolitho2, Caroline Kambuggu Nabasirye3, Marvin Musinguzi2, Raymond Tumwesigye3, Everlyne Achan2 and Amir Kabunga4
1Department of Environmental Health and Disease Control, Lira University, Lira, Uganda
2Department of Community Health, Lira University, Lira, Uganda
3Department of Nursing, Lira University, Lira, Uganda
4Department of Psychiatry, Lira University, Lira, Uganda
- *Corresponding Author:
- Eustes Kigongo
Department of Environmental Health and Disease Control,
Lira University,
Lira,
Uganda
Tel: 0770681031
E-mail: ekigongo@lirauni.ac.ug
Received date: March 24, 2023, Manuscript No. IPJCS-23-16148; Editor assigned date: March 28, 2023, PreQC No. IPJCS-23-16148 (PQ); Reviewed date: April 12, 2023, QC No. IPJCS-23-16148; Revised date: May 25, 2023, Manuscript No. IPJCS-23-16148 (R); Published date: June 02, 2023, DOI: 10.4172/2471-9749.8.1.003
Citation: Kigongo E, Anyolitho MK, Nabasirye CK, Musinguzi M, Tumwesigye R, et al. (2023) Factors Influencing Utilization of Modern Contraceptive Methods among Rural Youths in Northern Uganda. J Reproduct Health Contracept Vol:8 No:1.
Abstract
Background: Reducing unwanted pregnancies is a top priority of the international community and an important prerequisite in the achievement of several sustainable development goals. Men and women of reproductive age brackets need to be provided with and use contraceptives so that they are able to prevent such unwanted pregnancies. Hoverer, utilization of modern contraceptive products especially among young people is reported to be very low, even in nations where such products are widely available and free. Thus, we set out to assess the factors influencing the utilization of modern contraceptive methods among rural youths in Lira district of Lango sub region, Northern Uganda.
Materials and methods: This was a community based cross sectional study conducted between August and November 2022. Data was collected using interviewer administered questionnaire among randomly selected 533 youths aged 15 to 24 years. Analysis was performed using STATA 17. Descriptive statistics were used to summarize the data collected. Bivariate analysis was done by running the Pearson chi-square at 95% confidence intervals. Multivariate analysis was performed, and prevalence ratios with a 95% confidence interval were reported through a modified Poisson regression model with robust variance estimation. Variables with p ≤ 0.05 were considered to be statistically significant with the outcome variable.
Results: A total of 533 questionnaires were filled generating a response rate of 92.4% with a mean age of 17.6 (± 2.4) years. The majorities were females 345 (64.7%) and had attained secondary education 232 (43.5%). Most of the youths 361 (67.7%) were students who were living with their parents 359 (67.3%) and 215 (40.3%) Anglicans. Only more than one third of the youths (192:36%) were utilizing modern contraceptives. Almost two third of the respondents (333:62.5%) did not have enough privacy at the health facilities and almost one third (175:32.8%) had sexual and reproductive health challenges. The predictors of modern contraceptive methods used were being aged 18 to 19 years (APR: 1.20; 95% CI: 1.09-1.42; p=0.03), living with parents (APR: 0.79; 95% CI: 0.66-0.93, p=0.006) and facing MCM challenges (APR: 1.22; 95% CI: 1.04-1.44, p=0.02).
Conclusion: There is a relatively low utilization of modern contraceptive methods among the youth in rural northern Uganda. Older youth who are living with parents and facing sexual reproductive health problems are likely to use modern contraceptives compared to the young ones who do not live with their parents. There is a dire need for deliberate efforts directed at ensuring that young people in northern Uganda access and utilise modern contraceptive services to avert the rising cases of unwanted pregnancies in the formerly ravaged Northern insurgency.
Keywords
Family planning; Modern contraceptive methods; Youth; Implants; Sterilization; Intrauterine devices
Introduction
Globally, approximately 40% of pregnancies are unplanned, 43% of the pregnancies in the global south are unintended and 84% of those occur in women with an unmet need for reliable contraceptives [1]. The youth in low and mid income counties have close to 21 million pregnancies each year, of which about 50% are unplanned and which results in 12 million birth [2]. If all unmet needs for contraception were satisfied in low income nations, unplanned births may decline by an estimated three quarters and maternal mortality by a third [3]. Additionally, there are a host of international efforts to minimize the global unmet demand.
Reducing unwanted pregnancies is a top objective for the international community and the wide ranging advantages of contraception are related to several of the sustainable development goals [4]. Effective contraception use among youth is predicted to lower unexpected pregnancies by 59%, unplanned births by 62%, abortion by 57% and abortion of undesired pregnancies by 71% [5]. Additionally, it is possible to prevent close to 32% of maternal deaths, 90% of abortion related deaths and 20% of pregnancy related morbidity and mortality. Although there are now many different types of modern contraceptive products, there is underutilization of these products especially among the youth even in nations where it is widely available and free. Thus, to achieve this goal, there is a need to understand the factors influencing the utilization of modern contraceptive methods.
Studies in West Africa and Bangladesh indicate that youth in rural areas had significantly lower utilization of modern contraception than youth in urban areas [6,7]. Despite improvements in SRH access in East African countries including Uganda, there are still significant gaps in the SRH service availability, utilization and quality, and there remains a significant unmet need for contraception, especially among the youth [8]. There is limited information on modern contraceptive use among youth in rural settings in Uganda. Most of the available literature is on women in general and mostly in urban areas [9]. There is a need for youth focused studies in a rural setting to formulate evidence based policies to enhance the utilization of modern contraceptives. Therefore, this study assessed the factors influencing the utilization of modern contraceptive methods among rural youth in Northern Uganda.
Materials and Methods
Study area and setting
The study was conducted in Lira district, located in the Northern region of Uganda. It is the main administrative and commercial center of Lango sub region. According to projections of 2020 by the Uganda bureau of Statistics (UboS) based on the 2014 population census, the district had approximately 474,200 people with predominantly the Lango tribe. It has two divisions, East and West with each division comprising wards and cells. The district consists of many health facilities including Ogur health centre IV and Amach health centre IV, among other health centres IIIs IIs, and private health facilities, clinics, and drug shops providing reproductive health services.
Study design
The study adopted a community based cross sectional design using quantitative approaches to data collection and analysis. It was conducted between August and November 2022 in Lira district. The cross sectional design was used because it allows assessment of cause and effect at a single point in time.
Study participants and sample selection
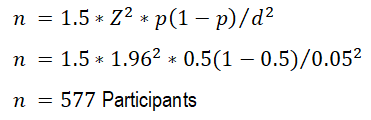
The study was conducted among young people. Youths were defined as any boy or girl from 15 to 24 years. According to the national health statistics, people aged 15 to 24 years have a disproportionate burden of sexual and reproductive health risks and are therefore a key population [10]. The sample size for the study was determined using the Kish Leslie formula for cross sectional studies [11]. Given that no recent study has been conducted to ascertain the level of modern contraceptive use among this group, a proportion (p) of 50% was used to obtain the maximum sample size. A-Z value of 1.96 and an error margin (d) of 5% were used in the calculation. Given that cluster sampling was used, a design effect of 1.5 was based on similarly conducted studies.
Sampling criteria
Respondents were selected using multistage random sampling procedure with clustering at the divisions. The district is divided into East and South constituencies all of which were involved for representativeness. Both divisions, east and west were used for representativeness. From each constituency 2 wards were selected and from each ward 2 cells were selected using a simple random sampling procedure. Households were selected consecutively with the help of the local council one for each of the participating cells. All households with young people aged 15 to 24 years were approached with one person selected from each household, for those that had more than one young person.
Data collection and analysis
Data was collected using structured interviewer administered questionnaires. The questionnaire was designed based on literature from similar studies, prepared in English and then translated to Iuo, the native language used in the study area [12,13]. The questionnaire was pretested among 57 randomly selected young people from Aber sub-county in Oyam district. The dependent variable for the study was the utilization of modern contraceptives use among young people (15 to 24 years), measured as a binary outcome of yes or no for those who had used any of the modern contraceptive methods or not. The methods include injectables, implants, sterilization, Intrauterine Devices (IUDs), condoms, spermicides, diaphragms and cervical caps. The independent variables include the socio demographic characteristics of respondents and hindrances in the utilization of modern contraceptive methods from the health facilities available. Five research assistants with at least a diploma in social sciences or related fields were recruited and trained in the study and data collection. Data collected was entered in to Microsoft Excel worksheet software and thereafter cleaned. The data was then exported to STATA version 17 for subsequent analysis. Descriptive statistics were used to summarize the data collected. Bivariate analysis was done by running the Pearson chi-square at 95% confidence intervals. Significant variables were considered at a p-value of 0.05; these were considered for multivariate analysis. At multivariate analysis, prevalence ratios with a 95% confidence interval were reported through a modified Poisson regression model with robust variance estimation. Odds ratios could not be used as estimates because they would overestimate the effect due to the high prevalence (36%) of the primary outcome. Variables with p ≤ 0.05 was considered to be statistically significant with the outcome variable.
Results
Sociodemographic characteristics of young adults
A total of 533 out of the 577 respondents fully answered the questions generating a response rate of 92.4%. Respondents had a mean age of 17.6 (± 2.4) years. The majorities were females 345 (64.7%) and had attained secondary education 232 (43.5%). Only 96 (18%) of the respondents reported that were in a marital relationship and 155 (29.1%) lived in rural areas, 359 (67.3%) were living with their parents, 361 (67.7%) were students and 215 (40.3%) were Anglicans. Also, results show that 192 (36%) were utilizing modern contraceptives, more than a quarter 175 (32.8%) faced sexual and reproductive health challenges and 333 (62.5%) did not have enough privacy at the health facilities (Table 1).
| Characteristic | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Age | 15-17 | 292 | 54.8 |
| 18-19 | 179 | 33.6 | |
| 20-24 | 62 | 11.6 | |
| Gender | Female | 345 | 64.7 |
| Male | 188 | 35.3 | |
| Education | None | 52 | 9.8 |
| Primary | 200 | 37.5 | |
| Secondary | 232 | 43.5 | |
| Tertiary | 49 | 9.2 | |
| Engaged in a sexual relationship | No | 437 | 82 |
| Yes | 96 | 18 | |
| Mothers education | None | 114 | 21.4 |
| Primary | 207 | 38.8 | |
| Secondary | 154 | 28.9 | |
| Tertiary | 58 | 10.9 | |
| Fathers education | None | 56 | 10.5 |
| Primary | 135 | 25.3 | |
| Secondary | 177 | 33.2 | |
| Tertiary | 165 | 40 | |
| Residence | Rural | 155 | 29.1 |
| Urban | 378 | 70.9 | |
| Religion | Anglican | 215 | 40.3 |
| Catholic | 201 | 37.7 | |
| Muslim | 62 | 11.6 | |
| Other | 55 | 10.3 | |
| Living with parents | No | 174 | 32.7 |
| Yes | 359 | 67.3 | |
| Employment | Formal employed | 19 | 3.6 |
| Self-employed | 69 | 13 | |
| Student | 361 | 67.7 | |
| Unemployed | 84 | 15.8 | |
| Faced SRH challenges | No | 358 | 67.2 |
| Yes | 175 | 32.8 | |
| No staff of same gender | No | 448 | 84.1 |
| Yes | 85 | 15.9 | |
| Mistreated by staff | No | 338 | 63.4 |
| Yes | 195 | 36.6 | |
| Not enough privacy | No | 200 | 37.5 |
| Yes | 333 | 62.5 | |
| Fear embarrassment | No | 324 | 60.8 |
| Yes | 209 | 39.2 | |
| Difficult to get to the health facility | No | 409 | 76.6 |
| Yes | 124 | 23.3 | |
| Long waiting time | No | 462 | 86.7 |
| Yes | 71 | 13.3 |
Table 1: Characteristics regarding modern contraceptive service utilization among young people in city, 2022.
Factors associated with the utilization of modern contraceptive methods
From the bivariate analysis in Table 2, the age of the respondent (X2=108.648; p<0.001), education level (X2=56.765; p<0.001), marital relationship (X2=151.475; p<0.001), parents education (X2=21.457; p<0.001), residence (X2=13.025; p<0.001), religion (X2=9.025; p=0.03), living with parents (X2=153.174; p<0.001), employment status (X2=125.194; p<0.001), faced SRH challenges (X2=124.014; p<0.001), mistreated by hospital staff (X2=15.117; p<0.001) and difficulty in reaching the health facility (X2=3.971; p=0.05)were associated with utilization of modern contraceptive methods.
| Characteristic | MCM utilization | X2 | P value | |
|---|---|---|---|---|
| No n=341 (64%) | Yes n=192 (36%) | |||
| Age | ||||
| 15-17 | 243 (71.3) | 49 (25.5) | 108.648 | <0.001* |
| 18-19 | 80 (23.5) | 99 (51.6) | ||
| 20-24 | 18 (5.3) | 44 (22.9) | ||
| Gender | ||||
| Female | 219 (64.2) | 126 (65.6) | 0.106 | 0.75 |
| Male | 122 (35.8) | 66 (34.4) | ||
| Education | ||||
| None | 19 (5.6) | 33 (17.2) | 56.765 | <0.001* |
| Primary | 155 (45.5) | 45 (23.4) | ||
| Secondary | 152 (44.6) | 80 (41.7) | ||
| Tertiary | 15 (4.4) | 34 (17.7) | ||
| Engaged in a sexual relationship | ||||
| No | 332 (97.4) | 105 (54.7) | 151.475 | <0.001* |
| Yes | 9 (2.6) | 87 (45.3) | ||
| Mothers education | ||||
| None | 74 (21.7) | 40 (20.8) | 21.457 | <0.001* |
| Primary | 110 (32.3) | 97 (50.5) | ||
| Secondary | 118 (34.6) | 36 (18.8) | ||
| Tertiary | 39 (11.4) | 19 (9.9) | ||
| Fathers education | ||||
| None | 35 (10.3) | 21 (10.9) | 16.446 | 0.001* |
| Primary | 71 (20.8) | 64 (33.3) | ||
| Secondary | 132 (38.7) | 45 (23.4) | ||
| Tertiary | 103 (30.2) | 62 (32.3) | ||
| Residence | ||||
| Rural | 81 (23.8) | 74 (38.5) | 13.025 | <0.001* |
| Urban | 260 (76.3) | 118 (61.5) | ||
| Religion | ||||
| Anglican | 139 (40.8) | 76 (39.6) | 9.025 | 0.03* |
| Catholic | 127 (37.2) | 74 (38.5) | ||
| Muslim | 32 (9.4) | 30 (15.6) | ||
| Other | 43 (12.6) | 12 (6.3) | ||
| Living with parents | ||||
| No | 47 (13.8) | 127 (66.2) | 153.174 | <0.001* |
| Yes | 294 (86.2) | 65 (33.8) | ||
| Faced SRH challenges | ||||
| No | 287 (84.2) | 71 (37.0) | 124.014 | <0.001* |
| Yes | 54 (15.8) | 121 (63.0) | ||
| No staff of same gender | ||||
| No | 294 (86.2) | 154 (80.2) | 3.309 | 0.07 |
| Yes | 47 (13.8) | 38 (19.8) | ||
| Mistreated by staff | ||||
| No | 237 (69.5) | 101 (52.6) | 15.117 | <0.001* |
| Yes | 104 (30.5) | 91 (47.4) | ||
| Not enough privacy | ||||
| No | 124 (36.4) | 76 (39.6) | 0.543 | 0.46 |
| Yes | 217 (63.6) | 116 (60.4) | ||
| Fear embarrassment | ||||
| No | 217 (63.6) | 107 (55.7) | 3.222 | 0.07 |
| Yes | 124 (36.4) | 85 (44.3) | ||
| Difficult to get to the health facility | ||||
| No | 271 (79.5) | 138 (71.9) | 3.971 | 0.05* |
| Yes | 70 (20.5) | 54 (28.1) | ||
| Long waiting time | ||||
| No | 301 (88.3) | 161 (83.9) | 2.074 | 0.15 |
| Yes | 40 (11.7) | 31 (16.2) | ||
| Note: X2: Chi-square value; *significant variable (P ≤ 0.05) | ||||
Table 2: Bivariate analysis for modern contraceptive service utilization among young people in city, 2022.
Predictors of utilization of modern contraceptive methods
Table 3 shows that being aged 18 to 19 years (APR: 1.20; 95% CI: 1.09-1.42; p=0.03), living with parents (APR: 0.79; 95% CI: 0.66-0.93, p=0.006) and facing MCM challenges (APR: 1.22; 95% CI: 1.04-1.44, p=0.02) had statistically significant association with utilization of MCM. Young people aged 18 to 19 years were 1.2 times more likely to utilize SRH services compared to their counterparts below 18 years. Young people living with their parents were less likely to utilize MCMs compared to those living alone. Those who faced MCMs challenges were 1.22 times more likely to utilize MCM services compared to those who did not face challenges.
| Factor | MCM utilization | Crude PR (95% CI) | Adjusted PR (95% CI) | P value | |
|---|---|---|---|---|---|
| No n (%) | Yes n (%) | ||||
| Age | |||||
| 15-17 | 243 (71.3) | 49 (25.5) | Ref | ||
| 18-19 | 80 (23.5) | 99 (51.6) | 1.32 (1.14-1.56)*** | 1.20 (1.09-1.42) | 0.03 |
| 20-24 | 18 (5.3) | 44 (22.9) | 1.46 (1.18-1.82)** | 1.17 (0.92-1.48) | 0.21 |
| Education | |||||
| Living with parents | |||||
| No | 47 (13.8) | 127 (66.2) | Ref | 0.006 | |
| Yes | 294 (86.2) | 65 (33.8) | 0.68 (0.59-0.79)*** | 0.79 (0.66-0.93) | |
| Faced MCM challenges | |||||
| No | 287 (84.2) | 71 (37.0) | Ref | 0.02 | |
| Yes | 54 (15.8) | 121 (63.0) | 1.41 (1.22-1.64)*** | 1.22 (1.04-1.44) | |
| Note: PR: Prevalence Risk ratio; *** p<0.01, ** p<0.05, * p<0.1; CI: Confidence Interval | |||||
Table 3: Multivariate analysis for modern contraceptive service utilization among young people in Lira city, 2022.
Discussion
In our study, we assessed the factors influencing the utilizing modern contraceptive methods among the youth aged 15 to 24. We found the overall utilizing modern methods among young adults aged 175 (32.8%). Our results show that being aged 18 to 19 years (APR: 1.20; 95% CI: 1.09-1.42; p=0.03), living with parents (APR: 0.79; 95% CI: 0.66-0.93, p=0.006), and facing sexual reproductive health problems (APR: 1.22; 95% CI: 1.04-1.44, p=0.02) had statistically significant association with utilization of MCM. This low level of utilization suggests that the use of modern contraceptives for fertility prevention is still a problem among youth in rural northern Uganda. Our finding resonates with that of Yaha and colleagues who reported low contraceptive use in many Sub-Saharan African countries [14]. However, the 32.8% observed in this study is higher than the 18.0% reported in Ghana and 19.0% in Congo [15]. This discrepancy might be because of the elapsed study period and the small sample size in the previous studies.
Our results show that youth aged 18 to 19 years were 1.2 times more likely to utilize MCM services compared to their counterparts below 18 years. The lower contraceptive use might be because youth aged below 18 years are still in school and due to that might not want to have children to disrupt their education [16]. Additionally, youth aged 18 to 19 years are highly sexually active, thus, utilizing modern contraception to avoid unintended pregnancies [17]. Our results are in line with findings of other studies showing that age was associated with modern contraceptive use [18,19].
Those who faced sexual reproductive health problems were 1.22 times more likely to utilize MCM services compared to those who did not face challenges. In this study, the challenges faced included Sexually Transmitted diseases (STIs), unintended pregnancy, and abortion. The results suggest the youth became aware that some modern contraceptive methods help to prevent the transmission of STIs [20]. Also, the youth may have realized after facing such challenges that modern contraceptive methods have clear benefits including the prevention of unwanted pregnancies and abortion.
Conclusion
The present study found a relatively low utilization of modern contraceptive methods among the youth in rural Northern Uganda and the associated factors were age, living with parents and facing sexual reproductive health problems. There is a need to further enlighten the youth in rural areas on the need to utilize modern contraceptive methods.
Strengths and Limitations
The study’s sample size is large enough and therefore the results may be generalized to other similar populations. Secondly, this study was conducted in a rural setting adding to the limited literature in such settings. This study however has its limitations: The data is based on a cross sectional sample and may not be representative of all the youth rural areas in Uganda. Also, data collection was conducted in private locations and participants were assured of confidentiality, self-reported tools were used to collect data which could have produced social desirability biases in responses.
Ethical Approval
The study was approved by the Gulu University Research and Ethics Committee (GUREC-2022-329). Introductory letters from Lira university were taken to the District Health Officer (DHO) who approved the study to be conducted in Lira district. An informed consent form was administered before data collection to all respondents 18 years and above and assent forms and consent forms for parents and children aged 15 to 17 years respectively.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgement
The authors wish to acknowledge all study participants.
Authors’ Contribution
All authors made significant contribution to the work reported, whether that is in the conception, study design, reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Conflict of Interest
Authors have no conflict of interest.
Funding
No funding.
References
- D’Souza P, Bailey JV, Stephenson J, Oliver S (2022) Factors influencing contraception choice and use globally: A synthesis of systematic reviews. Eur J Contracept Reprod Health Care 27:364–372
[Crossref] [Google Scholar] [PubMed]
- Ahmed S, Li Q, Liu L, Tsui AO (2012) Maternal deaths averted by contraceptive use: An analysis of 172 countries. The Lancet 380:111–125
[Crossref] [Google Scholar] [PubMed]
- O’Regan A, Thompson G (2017) Indicators of young women’s modern contraceptive use in Burkina Faso and Mali from demographic and health survey data. Contracept Reprod Med 2:1-8
[Crossref] [Google Scholar] [PubMed]
- Kawuki J, Gatasi G, Sserwanja Q, Mukunya D, Musaba MW (2022) Utilisation of modern contraceptives by sexually active adolescent girls in Rwanda: A nationwide cross-sectional study. BMC Womens Health 22:1–10
[Crossref] [Google Scholar] [PubMed]
- Namasivayam A, Lovell S, Namutamba S, Schluter PJ (2020) Predictors of modern contraceptive use among women and men in Uganda: A population level analysis. BMJ Open 10:e034675
[Crossref] [Google Scholar] [PubMed]
- Kaniki FR (2019) Factors influencing the use of modern contraceptive methods among rural women of child bearing age in the democratic republic of the Congo. J Family Med Prim Care 8:2582-2586
[Crossref] [Google Scholar] [PubMed]
- Asiimwe JB, Ndugga P, Mushomi J, Manyenye Ntozi JP (2014) Factors associated with modern contraceptive use among young and older women in Uganda: A comparative analysis. BMC Public Health 14:1-1
[Crossref] [Google Scholar] [PubMed]
- Yaya S, Uthman OA, Ekholuenetale M, Bishwajit G (2018) Women empowerment as an enabling factor of contraceptive use in Sub-Saharan Africa: A multilevel analysis of cross-sectional surveys of 32 countries. Reprod Health 15:1–12
[Crossref] [Google Scholar] [PubMed]
- Apanga PA, Adam MA (2015) Factors influencing the uptake of family planning services in the Talensi district, Ghana. Pan Afr Med J 20
[Crossref] [Google Scholar] [PubMed]
- Adebowale SA, Adeoye IA, Palamuleni ME (2013) Contraceptive use among Nigerian women with no fertility intention: Interaction amid potential causative factors. Afr Pop Stud 27:127-139
- Ba DM, Ssentongo P, Agbese E, Kjerulff KH (2019) Prevalence and predictors of contraceptive use among women of reproductive age in 17 Sub-Saharan African countries: A large population based study. Sex Reprod Healthc 21:26-32
[Crossref] [Google Scholar] [PubMed]
- Guta A, Amsalu B, Weldamanuel T, Sema A, Abera L, et al. (2021) Utilization of modern contraceptives and associated factors among street women in Dire Dawa, Eastern Ethiopia: A mixed study. Reprod Health 18:1-2
- Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, et al. (2011) Implementation of goal directed therapy for children with suspected sepsis in the emergency department. Pediatrics 127:e758-e766
[Crossref] [Google Scholar] [PubMed]
- Hermansen CL, Mahajan A (2015) Newborn respiratory distress. Am Fam Physician 92:994-1002
[Google Scholar] [PubMed]
- Butt W, MacLaren G (2007) Extracorporeal membrane oxygenation and sepsis. Crit Care Resusc 9:76-80
[Google Scholar] [PubMed]
- Goldstein B, Giroir B, Randolph A (2005) International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6:2-8
- Emr BM, Alcamo AM, Carcillo JA, Aneja RK, Mollen KP (2018) Pediatric sepsis update: How are children different?. Surg Infect (Larchmt) 19:176-183
[Crossref] [Google Scholar] [PubMed]
- Shane AL, Sanchez PJ, Stoll BJ (2017) Neonatal sepsis. The lancet 390:1770-1780
[Crossref] [Google Scholar] [PubMed]
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, et al. (2002) Late onset sepsis in very low birth weight neonates: The experience of the NICHD neonatal research network. Pediatrics 110:285-291
[Crossref] [Google Scholar] [PubMed]
- Wynn JL, Wong HR, Shanley TP, Bizzarro MJ, Saiman L, et al. (2014) Time for a neonatal specific consensus definition for sepsis. Pediatr Crit Care Med 15:523-528
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
