Diagnostic Studies, Complications and Treatment Results in Children with Cholelithiasis
Nesrin C, Kaan D, Ayhan D, Saadet D and Nihat D
Nesrin C1*, Kaan D2, Ayhan D1, Saadet D3 and Nihat D1
1Department of Pediatrics, Faculty of Medicine, University of Yuzuncu Yil, Van, Turkey
2Department of Pediatric Gastroenterology, Faculty of Medicine, University of Yuzuncu Yil, Van, Turkey
3Department of Pediatrics, Lokman Hekim Hospital, Van, Turkey
- *Corresponding Author:
- Nesrin C
Department of Pediatrics
Faculty of Medicine
University of Yuzuncu Yi
Van, Turkey
Tel: 05324318522
Email: drnesrinceylan@hotmail.com
Received Date: April 18, 2016 Accepted Date: April 22, 2016 Published Date: April 29, 2016
Copyright: © 2016 Nesrin C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objectives: The aim of this present study is to evaluate the characteristics of the child patients with cholelithiasis, underlying predisposing factors, complications, and the responses to ursodeoxycholic acid (UDCA) treatment.
Patients and Methods: 68 child patients applied to the pediatric gastroenterology clinic due to cholelithiasis were examined for approximately 2, 5 years. The data about the patients were collected from the outpatient file records retrospectively average values of the groups were compared using T-test.
Results: The average age of the patients was 7.5 ± 5 years (range: 1 month - 18 years), and 54.4% were male. The most common initial complaints of patients were abdominal pain (58.8%). 8.8% of patients had used ceftriaxone. Hemolytic disease was found in 1 patient (1.5%). A family history existed in 4.4% of the patients. In ultrasonography, hyperechoic image in gallbladder was evaluated as calculus in 82.4% of patients and as sludge in 17.6% of patients. The stone size was measured 6.9 ± 3.6 mm (range 3-15 mm) in average. 2.9% of patients had cholecystitis, 1.5% had acute pancreatitis and 1.5% had chronic pancreatitis. With magnetic resonance cholangiopancreatography, choledochal cyst was detected in 2 patients, pancreas divisium in 1 patient, and duodenal duplication cyst in 1 patient. Ursodeoxycholic acid was started for all patients and continued for an average of 3.7 ± 3.4 months. It was observed that hyperechoic image disappeared in 34.1%, and did not improve in 65.9% of the 44 followed patients. 57.1% of the recovered patients were of those evaluated as sludge. Blood leucocyte and platelet counts of the patients with improved cholelithiasis, in the first application were significantly higher than those unimproved (p < 0.05). One of the patients was operated due to cholecystectomy and another due to duodenal duplication cyst.
Conclusions: Cholelithiasis began to be frequently identified in children. With the diagnosis cholelithiasis, an underlying hemolytic disease can be diagnosed or anatomical defect associated with biliary tract can be detected. Although treatment success with UDCA at various rates has been reported, it is a safe, easy and inexpensive treatment option in children.
Keywords
Cholelithiasis; Ursodeoxycholic acid; Pancreatitis; Ceftriaxone; Children
Introduction
Cholelithiasis is increasingly seen in children with the widely use of ultrasonography [1-4]. The prevalence in the society has been reported to be 0.13-1.9% in children and adolescents [1,5,6]. Although the use of antibiotics and hemolytic diseases are reported as the most common causes, it mostly remains idiopathic [1-4]. In the present study, the cases with cholelithiasis have been reviewed, and their different features as well as underlying predisposing factors have been investigated. At the same time, we aimed to assess the response to ursodeoxycholic acid [UDCA] treatment and the factors affecting this response.
Materials and Methods
Ethical permission was obtained from Yüzüncü Yil University Medical School Clinical Researches Ethics Committee (Approval number: 08.10.2015/06). The study included pediatric patients with cholelithiasis determined by ultrasonography in pediatric gastroenterology clinic between the dates 01/02/2013 and 25/06/2015. From the outpatient file records, together with the general characteristics of the patients retrospectively, height and weight percentiles, reasons for application, gastrointestinal symptoms, routine biochemistry and blood count values, studies about the possible underlying factors, ultrasonography findings, the application time and success rate of ursodeoxycholic acid treatment, total follow-up period of the patients, and data on whether surgery was made were recorded. Patients were given UDCA in the dose of 20 mg/kg/d. The average values of the groups were compared using t-test and the values [p < 0.05] were considered significant.
Results
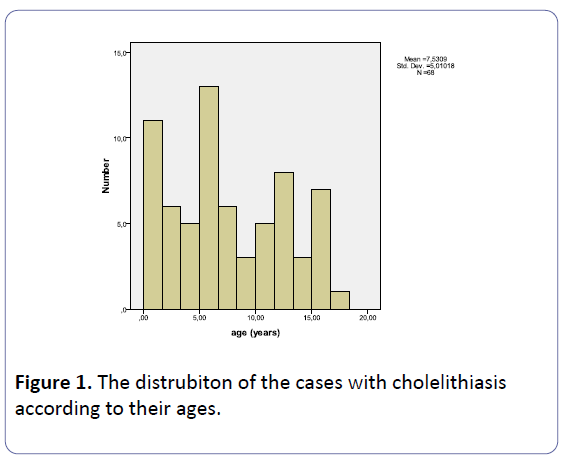
The average age of the 68 patients included in the study was 7.5 ± 5 years (range: 1 month - 18 years), and 54.4% were male (Figure 1). The most common initial complaints of patients were abdominal pain (58.8%). Weight percentile of 70.6% of patients and height percentile of 67.6% of patients ranged between 25-50. Body mass index (BMI) was found at an average of 17.2 ± 3.2. The presence of gallstones at the application to our clinic was known by families since 109 ± 240 days (range: 1-1100 days) before. A family history existed in 3 (4.4%) patients including a sister, a mother and a grandmother. Possible predisposing factors for patients are shown in Table 1.
Table 1: Possible predisposing factors in our cases n=68 with cholelithiasis.
| Predisposing factors | N |
|---|---|
| Medications | 9 |
| Ceftriaxone | 6 |
| Metformin | 1 |
| Factor VIII | 1 |
| Colchicine | 1 |
| Immune hemolytic anemia | 1 |
| Asthma | 1 |
| Chronic hepatitis B | 1 |
| Duchenne muscular dystrophy | 1 |
| Familial mediterranean fever | 1 |
| Hemophilia A | 1 |
| Cerebral palsy | 1 |
| Obesity | 1 |
| Chronic gastritis | 1 |
| Prematurity [total parenteral nutrition and use of different antibiotics] | 1 |
| Congenital CMV infection | 1 |
| Perinatal asphyxia [total parenteral nutrition and use of different antibiotics] | 1 |
| Type 1 diabetes mellitus | 1 |
| Pneumonia | 1 |
| Down syndrome | 1 |
In blood tests, hemoglobin was found as 13.2 g/dL ± 1.5, leucocyte as 8671/mL ± 2893, blood platelets as 331108/ml ± 109609, MCV as 80.2 fL ± 7, RDW as 14.2% ± 1.6, MPV 8 ± 0 9 fL, reticulocytes as 1.1% ± 0.4, ferritin as 52.7 ng/mL ± 69.7, ALT as 34 U/L ± 58, AST as 46 U/L ± 50, glycoside as 93 mg/dL ± 14, creatinine as 0.5 mg/dL ± 0.1, triglyceride as 116.6 mg/dL ± 61, cholesterol as 152.9 mg/dL ± 35.7, creatine kinase as 96 U/L ± 73, total bilirubin as 0.9 mg/dL ± 1.9, direct bilirubin as 0.5 mg/dL ± 1.4, amylase as 74.3 U/L ± 110.6, total protein as 7 g/dL ± 0.8, albumin as 4.3 g/dL ± 0.5, tissue transglutaminase IgA as 2.4 ± 2.3, antigliadin IgA as 2.7 ± 3.5, prothrombin time as 13.3 ± 1.3 s, partial thromboplastin time as 30.5 ± 7.5 s, INR as 1 ± 0.1, D-dimer as 1.5 ± 2.5, and fibrinogen 302 as 2 mg/dL ± 117.6.
In ultrasonography, hyperechoic image in gallbladder was evaluated as calculus in 82.4% of patients and as sludge in 17.6% of patients. Hyperechoic image was limited in the gallbladder at 92.6% of the patients. The number of stones in those considered as stone was one at 51.7%, and was more than one at 48.3%, the stone size in patients considered as calculus was measured 6.9 ± 3.6 mm (range 3-15 mm). In plain abdominal films, opacity was not observed in any patients. Ultrasonography also revealed hepatomegaly, choledochal cyst and polyps in the gallbladder one each patient. 2 patients had cholecystitis, 1 patient had acute pancreatitis and one patient had chronic pancreatitis. 14 (20.6%) patients were filmed by magnetic resonance cholangiopancreatography (MRCP). Choledochal cyst was detected in 2 patients, pancreas divisium in 1 patient, and duodenal duplication cyst in 1 patient.
Ursodeoxycholic acid was started for all patients and continued for an average of 3.7 ± 3.4 months. It was observed that hyperechoic image disappeared in 34.1%, and did not improve in 65.9% of the 44 followed patients. 57.1% of the recovered patients were of those evaluated as sludge. Blood leucocyte and platelet counts of the patients with improved cholelithiasis, in the first application were significantly higher than those unimproved (Table 2). One of the patients had cholecystectomy. Another case was operated due to chronic pancreatitis table and duodenal duplication cyst.
Table 2: Blood leukocyte and platelet values in cases with recovered and unrecovered cholelithiasis after ursodeoxycholic acid treatment.
| Cholelithiasis recovered | Cholelithiasis not recovered | p | |
|---|---|---|---|
| Blood leukocyte count [/mL] | 10509 | 8296 | <0.05 |
| Blood platelet count [/mL] | 434273 | 310093 | <0.05 |
Conclusion
Gallstones are being frequently detected in children with the common use of ultrasonography and are mostly recognized by ultrasonography performed for different reasons. Symptomatic cases are reported to be approximately 50% [2]. Khoo et al. [7] and Fakirullahoglu et al. [3] reported that it is seen in equal rates in girls, Dooki et al. [8] reported equal rates in males, and Bogue et al. [2] reported equal rates in males and females. In our study, the number of male patients was little more than the number of females. The average age is approximately 7 years as is in our study [1,2]. The reasons of cholelithiasis have not mostly been clarified. However, cholelithiasis may have very different reasons in childhood. Dooki et al. [8] reported the use of ceftriaxone as 27.3% and the incidence of hemolytic disease as 13.6% and reported 30.3% of patients with no predisposing factors. Tannuri et al. [9] and Muller et al. [10] reported hemolytic diseases in approximately 62% of patients being sent for surgery, and Walker et al. [4] reported hemolytic diseases in 15% of the patients.
Silva et al. [11] detected cholelithiasis in a ratio of 40.9% in children with sickle cell disease. Heide et al. [12] reported that 5.9% of obese children had cholelithiasis. They have stated that all these occurred when they lost more than 10% of their present weight when the diet. Similarly, Nunes et al. [13] stated that obese adolescents had cholelithiasis at the rate of 6.1%, and this is related to the rate of weight loss. Fradin et al. [14] have argued that cholelithiasis was a major risk factor for hospital stay in obese patients. Park et al. [15] reported that the prevalence of gallstones is significantly higher in patients with liver cirrhosis, and the related risk factors are diabetes, hypertriglyceridemia and severity of liver cirrhosis. Acalovschi et al. [16] argued that 1/3 of patients with cirrhosis have cholelithiasis, risk of complications due to surgery increases in severe liver disease and therefore medical treatment as much as possible is sound.
Nowadays, ceftriaxone induced gallstones are well known and are referred to as pseudolithiasis. In the use of ceftriaxone, Murata et al. [17] reported the presence of pseudolithiasis at the rate of 18.3%, and Rodríguez Rangel et al. [18] reported 42.5%. Rodríguez Rangel et al. [18] stated that stone size measured as 8 mm, and duration of resolution was 24.1 days, meanly. Koivusalo et al. [19] reported that children with cholesterol stone had low cholesterol absorbers with intact homeostasis of cholesterol metabolism, but children with black pigment stone had deteriorated cholesterol metabolism, and accumulation of cholestanol, campesterol and sitosterol in serum.
As the therapeutic strategies were extremely heterogeneous, conventional treatment for cholelithiasis is removing the gallstone with cholecystectomy. Surgical removal of gallstones in the causes of hemolytic anemia is often necessary. However, conservative approach is preferred in asymptomatic patients developing due to other reasons. For this, UDCA has been used frequently nowadays. UDCA reduces the biliary cholesterol saturation by inhibiting the absorption of cholesterol from intestines. Therefore, it is particularly effective in cholesterol-rich non-calcific stones [20]. UDCA treatment, especially in children with biliary sludge, is an alternative treatment to surgery. There is information available that UDCA shrinks the stones even though it does not completely remove them, prevents the growth and removes the symptoms [1,3,20].
Fakirullahoglu et al. [3] reported the gallstone resolution with UDCA at the rate of 32.3%, excluding patients who received ceftriaxone. In our study, 34% had improvement with UDCA and about half of these patients were evaluated as sludge. Gökçe et al. [21] reported that gallstone resolution with UDCA treatment was detected approximately 29.4% in symptomatic patients and they observed the resolution in 43.8% of children with ceftriaxone-associated gallstone. They proposed that the most important factor associated with gallstone resolution was to be an infant [<2 years of age] at the time of diagnosis. Della Corte et al. [1] applied UDCA treatment to 114 patients and observed dissolution of gallstones in only 8 of the patients. However, they determined symptomatic improvement in 65% of patients with UDCA and proposed that UDCA was ineffective in dissolution of gallstones but it had a positive effect on the symptoms.
Tannuri et al. [9] reported that 25.1% of patients with cholelithiasis have undergone surgeries due to the complications such as cholecystitis, and pancreatitis. Heide et al. [12] reported that cholecystectomy was performed in 22% of those in severely obese children with cholelithiasis. While 2 of our patients had cholecystitis, 1 had acute and 1 had chronic pancreatitis, 1 underwent surgery due to cholecystectomy, and 1 due to duodenal duplication cyst.
As a result, cholelithiasis began to be defined frequently in children and due to its symptoms and discontentment of surgical treatment, UDCA has been widely used. Although treatment success with UDCA at various rates has been reported, it is a safe, easy and inexpensive treatment option in children. With the diagnosis of cholelithiasis, an underlying hemolytic disease can be diagnosed and an anatomical defect associated with biliary tract can be detected. Therefore, the necessary examinations for etiology and advanced imaging with MRCP would be useful.
References
- Della Corte C, Falchetti D, Nebbia G, Calacoci M, Pastore M, et al. (2008) Management of cholelithiasis in Italian children: a national multicenter study. World J Gastroenterol 4: 383-388.
- Bogue CO, Murphy AJ, Gerstle JT, Moineddin R, Daneman A (200) Risk factors, complications, and outcomes of gallstones in children: a single-center review. J PediatrGastroenterolNutr 50: 303-308.
- Fakirullahoglu F, Dinler G, Kalayci AG (20) Cocuklukçagindasafrataslari: 60 olgunungeriyedönükincelenmesi. Turk Arch Ped 45: 9-23.
- Walker SK, Maki AC, Cannon RM, Foley DS, Wilson KM, et al. (203) Etiology and incidence of pediatric gallbladder disease. Surgery 54: 927-93.
- Kratzer W, Walcher T, Arnold F, Akinli AS, Mason RA, et al. (200) Gallstone prevalence and risk factors for gallstone disease in an urban population of children and adolescents. Z Gastroenterol 48: 683-687.
- Palasciano G, Portincasa P, Vinciguerra V, Velardi A, Tardi S, et al. (989) Gallstone prevalence and gallbladder volume in children and adolescents: an epidemiological ultrasonographic survey and relationship to body mass index. Am J Gastroenterol 84: 378-382.
- Khoo AK, Cartwright R2, Berry S3, Davenport M4 (204) Cholecystectomy in English children: evidence of an epidemic (997-202). J PediatrSurg 49: 284-288.
- Dooki MR, Norouzi A2 (203) Cholelithiasis in childhood: a cohort study in north of iran. Iran J Pediatr 23: 588-592.
- Tannuri AC, Leal AJ, Velhote MC, Gonlçalves ME, Tannuri U (202) Management of gallstone disease in children: a new protocol based on the experience of a single center. J PediatrSurg 47: 2033-2038.
- Muller CO, Boimond MB, Rega A, Michelet D, El Ghoneimi A, et al. (205) Safety and efficacy of one-stage total laparoscopic treatment of common bile duct stones in children. SurgEndosc 29: 83-836.
- Silva IV, Reis AF, Palare MJ, Ferrao A, Rodrigues T, et al. (205) Sickle cell disease in children: chronic complications and search of predictive factors for adverse outcomes. Eur J Haematol 94: 57-6.
- Heida A, Koot BG, Baan-Slootweg OH, PelsRijcken TH, Seidell JC, et al. (2014) Gallstone disease in severely obese children participating in a lifestyle intervention program: incidence and risk factors. Int J Obes (Lond) 38: 950-953.
- Nunes MM, Medeiros CC2, Silva LR3 (204) Cholelithiasis in obese adolescents treated at an outpatient clinic. J Pediatr (Rio J) 90: 203-208.
- Fradin K, Racine AD, Belamarich PF (204) Obesity and symptomatic cholelithiasis in childhood: epidemiologic and case-control evidence for a strong relation. J PediatrGastroenterolNutr 58: 02-06.
- Park JH, Kim TN, Lee SH (203) The prevalence and risk factors of gallstones in Korean patients with liver cirrhosis. Hepatogastroenterology 60: 46-465.
- Acalovschi M (204) Gallstones in patients with liver cirrhosis: incidence, etiology, clinical and therapeutical aspects. World J Gastroenterol 20: 7277-7285.
- Murata S, Aomatsu T2, Yoden A2, Tamai H2 (205) Fasting and bed rest, even for a relatively short period, are risk factors for ceftriaxone-associated pseudolitiasis. PediatrInt 57: 942-946.
- Rodríguez Rangel DA, PinillaOrejarena AP2, Bustacara Diaz M3, HenaoGarcía L3, LópezCadena A3, et al. (204) [Gallstones in association with the use of ceftriaxone in children]. An Pediatr (Barc) 80: 77-80.
- Koivusalo A, Pakarinen M2, Gylling H3, Nissinen MJ4,5 (205) Relation of cholesterol metabolism to pediatric gallstone disease: a retrospective controlled study. BMC Gastroenterol 5: 74.
- Guarino MP, Cocca S, Altomare A, Emerenziani S, Cicala M (203) Ursodeoxycholic acid therapy in gallbladder disease, a story not yet completed. World J Gastroenterol 9: 5029-5034.
- Gokce S1, Yildirim M, Erdogan D. (204) A retrospective review of children with gallstone: single-center experience from Central Anatolia. Turk J Gastroenterol 25: 46-53.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences