Abstract
POSTMENOPAUSAL BLEEDING AS A SYMPTOM OF ENDOMETRIAL ACTINOMYCOSIS IN THE ABSENCE OF INTRAUTERINE CONTRACEPTIVES AND WITH ALLERGY TO PENICILLIN
This case study focuses on a 66-year-old patient, allergic to penicillin, with endometrial actinomycosis, with no history of intrauterine contraceptive (IUD) administration, with symptomatology in the form of postmenopausal uterine bleeding and lower pelvic pain. Endometrial actinomycosis is an infection that occurs rarely, accompanied by non-specific symptomatology. The diagnosis is based on histological examination of affected tissue sample. The treatment is conducted with antibiotic therapy, administering high doses of intravenous antibiotics and, in certain cases, surgical treatment, as was the case in our patient.
Actinomycosis is a rare, chronic infectious disease caused by anaerobic, gram positive, filamentous microorganisms of the genus Actinomyces. The most commonly isolated species is Actynomices israeli (1). It is found as part of the normal flora of the human mouth, gastrointestinal and urogenital tracts. Healthy mucosa is a barrier against its spread in the body (2). The destruction of the mucosal barrier caused by traumas during endoscopic examinations, operations, or chronic inflammatory diseases is a predisposing factor for the development of actinomycosis. The disease occurs in several forms, the most common being cervicofacial, abdominal, and thoracic, while pelvic, generalized as well as localized on the CNS, are less common. (3, 4, 5, 6, 7,8) The uterus is relatively resistant to infections and endometrial infection is very rare. Genital infection is usually endogenous, possibly developed by direct spread through the abdomen, by ascending or inoculation, associated with IUDs, contaminated pessary, uterine prolapse, and criminal abortions (13) and it is difficult to make the diagnosis preoperatively. Endometrial Actynomucosis causes atypical symptoms such as abdominal pains, internal bleeding in genital organs, so it is difficult to determine the right diagnosis.The diagnosis of actinomycosis is most commonly made by isolating actinomycosis from a bioptate sample (9,10). In actinomycosis therapy, penicillin G is an option, in high doses and long-term use. Patients allergic to penicillin have been treated by tetracycline, clindamycin, erythromycin and cephalosporins (10, 11, 12). Surgical procedures are sometimes required. (9,10)
Author(s):
Tanja Petronijevic
Abstract | PDF
Share this

Google scholar citation report
Citations : 201
Journal of Reproductive Health and Contraception received 201 citations as per google scholar report
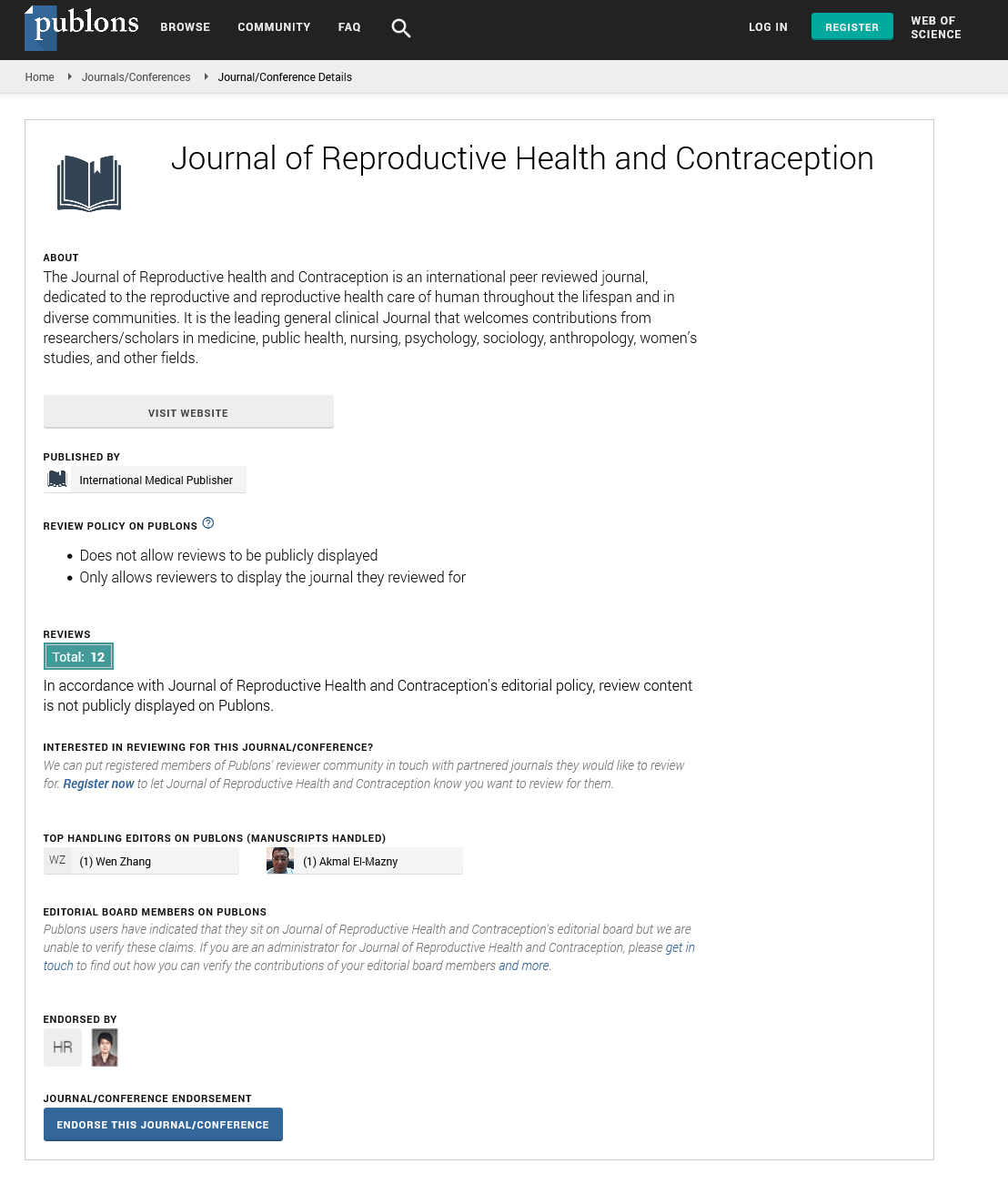
Journal of Reproductive Health and Contraception peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- WorldCat
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences