Abstract
Fertility sparing surgery in treatment of early stages of cervical cancer: The new standard of care?
Standard surgical approach to invasive cervical cancer carries risks of unfulfilled reproductive plans and morbidity, which could influence quality of life to a greater extent. Radical trachelectomy is a fertility sparing procedure with the aim to preserve reproductive potential of the patient with unchanged oncologic outcome. The procedure can be performed by vaginal or abdominal approach. Abdominal trachelectomy offers greater radicality concerning the parametrial resection with an easier learning curve, although studies demonstrate slightly lower reproductive success. Vaginal radical trachelectomy is combined with minimally invasive lymphadenectomy (laparoscopic or robotic). The procedure is applied to patients with early-stages of cervical cancer, FIGO staged as Ia1, Ia2 and smaller Ib1 tumours. Since the procedure is combined with an ex-tempore hystologic analysis, organization and experience of team is of crucial importance. Oncologic outcome is excellent and comparable to standard procedure. Fertility rates are between 40 and 70%, with increased rates of pregnancies achieved by assisted reproductive procedures (about 1/3). The rate of pregnancy complication is higher, and incude increased rates of abortions, preterm deliveries, chorioamnionitis and cesarean sections. In an attempt to further decrease morbidity and to optimise reproductive outcome, some institutions perform less radical approach – conisation or amputation of cervix, precedeed by pelvic lympadenectomy. Novel approaches include sentinel node biopsies and neoadjuvant chemotherapy followed by fertility sparing procedures. Since the oncologic safety of these procedures is yet to be determined, for now these procedures have to be considered as experimental. More studies, concerning the safety of above mentioned procedures, are needed, before they can fully be utilized in routine practice.
Author(s): Aleksandar Stefanovic
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 201
Journal of Reproductive Health and Contraception received 201 citations as per google scholar report
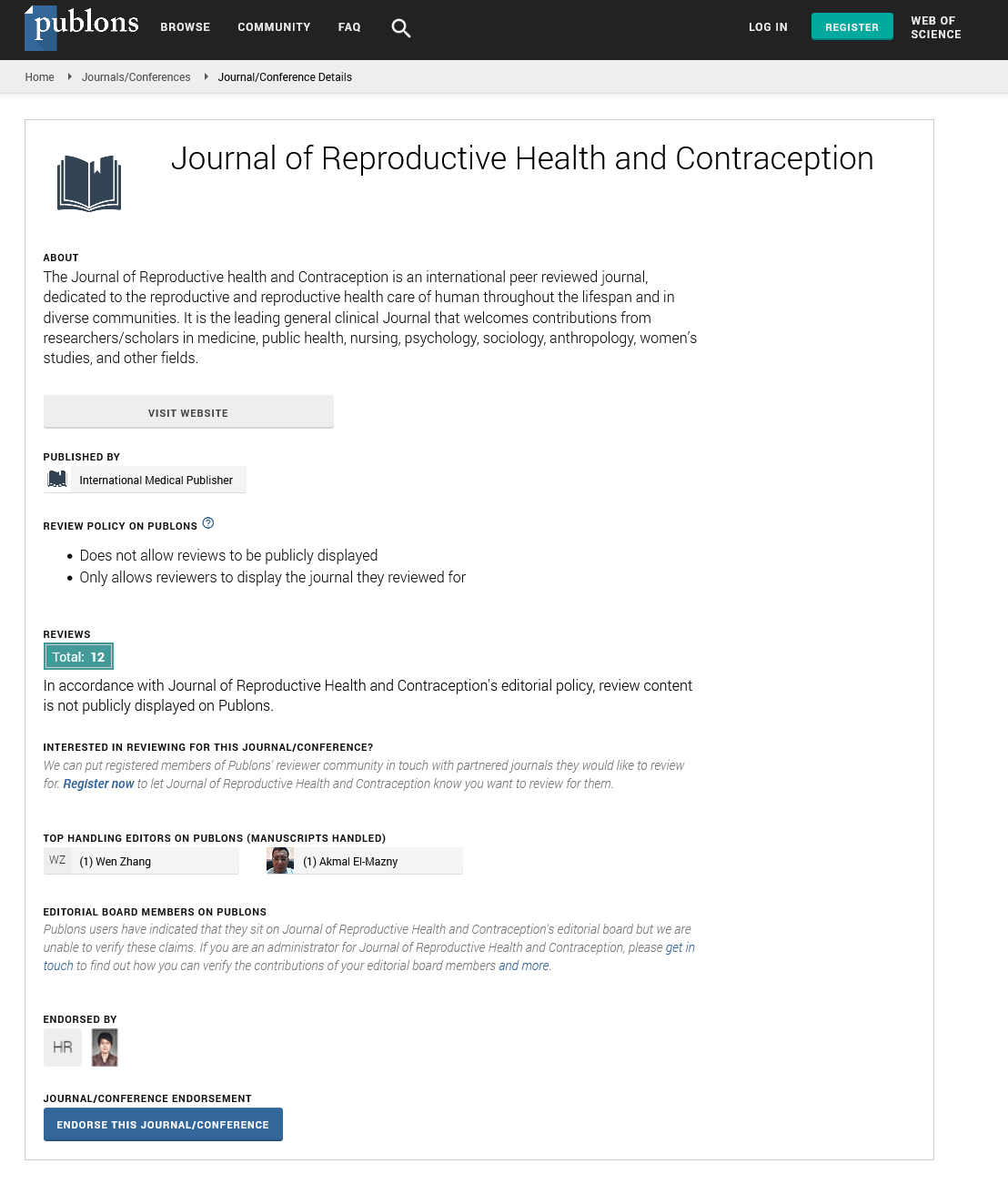
Journal of Reproductive Health and Contraception peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- WorldCat
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences