Abstract
Endometriosis hidden behind menopause, a new paradigm
Endometriosis is known to be an estrogen-dependent chronic inflammatory disease, classically characteristic of reproductive-age women. In postmenopausal patients it is a rare condition, reported to affect up to 2-5% of women worldwide. The pathophysiologic mechanisms responsible for either the exacerbation of previous undiagnosed disease or the development of de novo endometriotic lesions remain uncertain. Clinical presentation of endometriosis in postmenopausal women is very unspecific, ranging from asymptomatic to pelvic pain, ovarian cysts and to intestinal symptoms. To date, there are no specific biomarkers identified for the endometriosis diagnosis, even though inflammatory markers and CA-125 levels can be modified, highlighting the need for novel diagnostic biomarkers. Imaging techniques, such as ultrasound and magnetic resonance imaging can possibly diagnose endometriotic lesions; nevertheless a non-invasive accurate diagnostic method is not yet available. Due to difficulties in diagnosing endometriosis in postmenopausal women, laparoscopic surgery and biopsy of suspicious lesions is the gold standard for its definitive diagnosis, having the additional therapeutic potential. The use of menopausal hormone therapy in women with a history of endometriosis is controversial, and further studies are needed to outweigh its risks and benefits. Besides, the ideal therapeutic approach in de novo endometriosis is also not clarified for women after menopause. It is also believed that postmenopausal women with endometriosis have an increased risk for malignant tumours, apart from the ovarian cancer. This presentation pretends to summarize the main updates on the scarce literature related to endometriosis in postmenopausal women, which merits full medical attention.
Author(s): Mariana Robalo Cordeiro
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 201
Journal of Reproductive Health and Contraception received 201 citations as per google scholar report
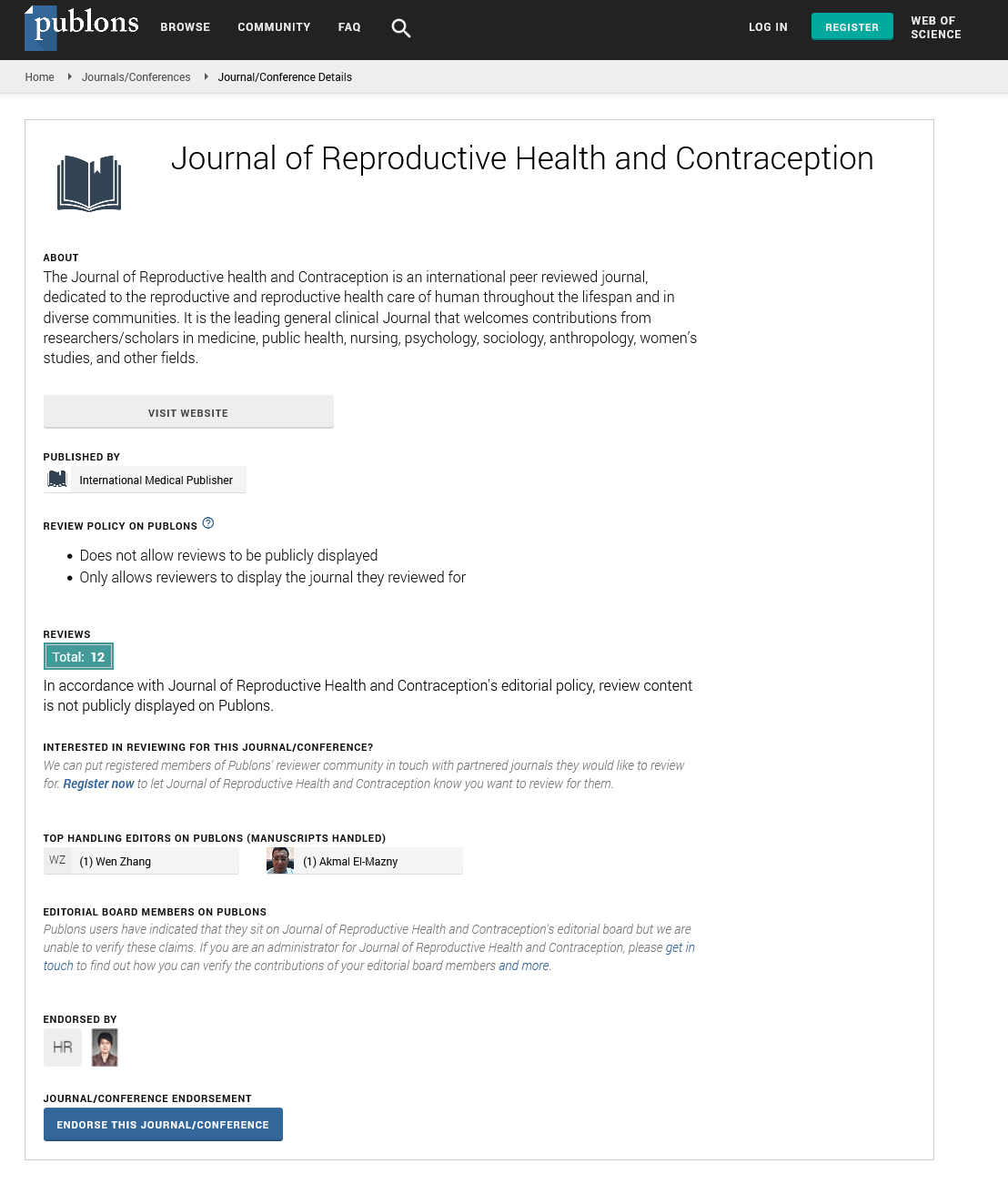
Journal of Reproductive Health and Contraception peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- WorldCat
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences