Abstract
AN EVALUATION OF EARLY INFANT DIAGNOSIS OF HIV AMONG INFANTS ATTENDING SELECTED LEVEL 4 AND LEVEL 5 HEALTH FACILITIES
Over 90% of HIV infections among children are through Mother-To-Child Transmission. The high rates of HIV infection among women, high birth rates and failure to utilize available Prevention of Mother-To-Child Transmission interventions translate to high rates of HIV transmission to children hence a high burden of paediatric HIV disease. The window of opportunity for effective intervention is short, many of these children often die very young from preventable and treatable common childhood illnesses. Many of them die of AIDS related causes before their HIV status is known hence not receiving the necessary interventions. Early diagnosis of HIV is therefore critical for timely intervention in order to save their lives, thus the need to scale up access to EID (early infant diagnosis of HIV) services. Progress in stopping new infections and ensuring that mothers are alive and healthy, requires reaching the full cross-section of pregnant women with essential health services, to achieve the vision 2030 of zero HIV infections and zero AIDS related deaths. Currently HIV infections of children born to HIV positive mothers is about 14%, this trend needs to be reversed. This study sought to find out EID utilization, its determinants and whether there is a difference in health outcome and HIV prognosis if EID is utilized at six weeks or diagnosis of HIV in children is done later. Mixed Methods Research Design was used in this study. That is QUAN-QUAL. Quantitative methods consisted of cross-sectional surveys and case-control. Qualitative methods used were focused group discussions and in-depth discussions.
Author(s):
BARSITO EMILY CHEMNGETICH RONO
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 201
Journal of Reproductive Health and Contraception received 201 citations as per google scholar report
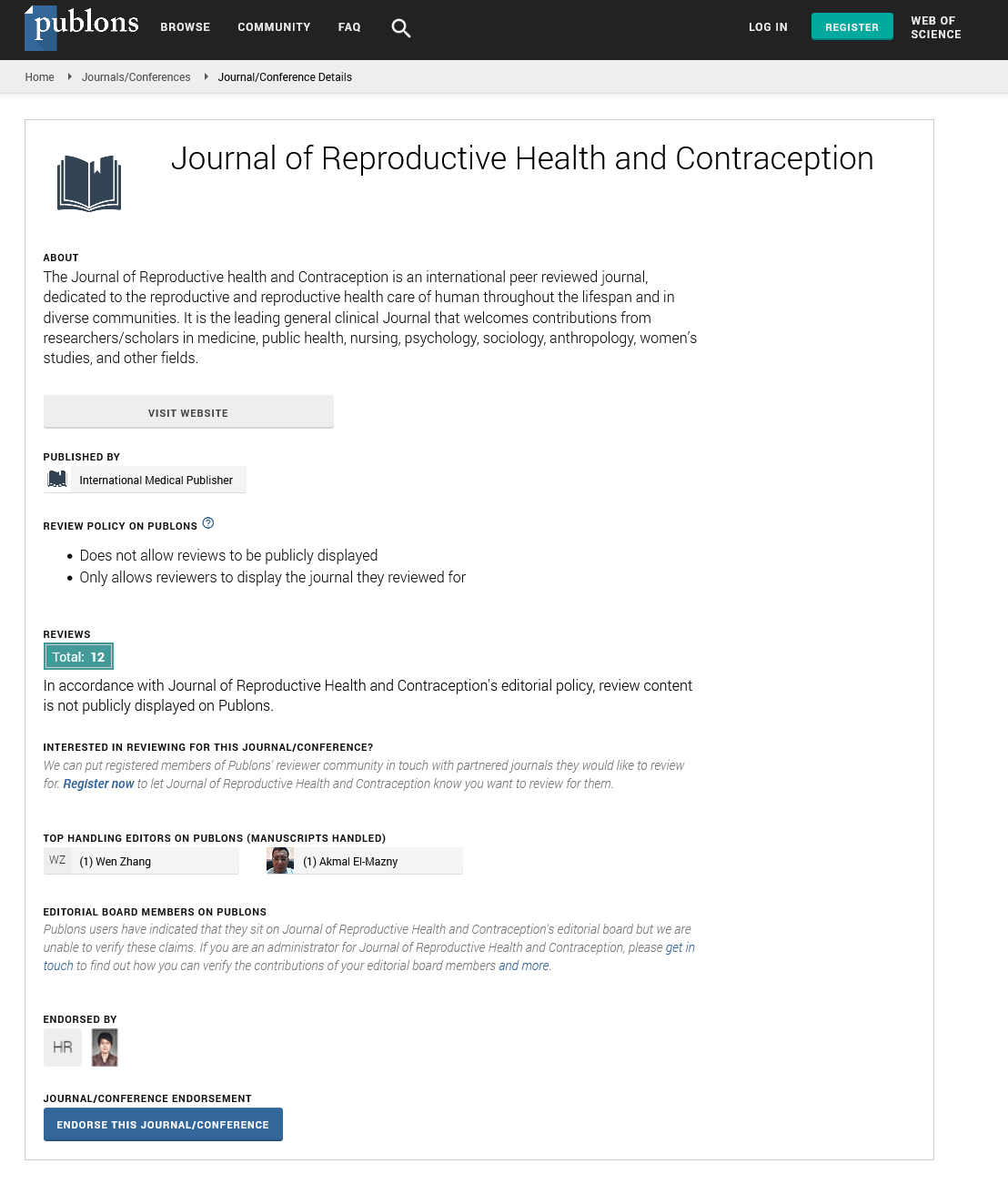
Journal of Reproductive Health and Contraception peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- WorldCat
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences